Iloperidone
Iloperidone, commonly known as Fanapt and previously known as Zomaril, is an oral atypical antipsychotic for the treatment of schizophrenia.
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Fanapt, Zomaril |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a609026 |
| License data |
|
| Routes of administration | Oral, injection |
| Drug class | Atypical antipsychotic |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 96% (oral; Tmax = 2–4 hours) |
| Protein binding | ~97% |
| Metabolism | Hepatic (CYP2D6-mediated hydroxylation and CYP3A4-mediated O-demethylation) |
| Elimination half-life | 18–33 hours |
| Excretion | urine (45.1–58.2%) and feces (19.9–22.1%) |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.106.441 |
| Chemical and physical data | |
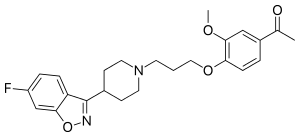
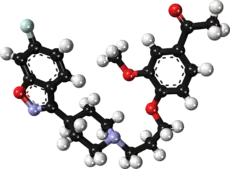
| Formula | C24H27FN2O4 |
| Molar mass | 426.488 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| | |
Medical uses
Iloperidone is indicated for the treatment of schizophrenia.[1] In a 2013 study in a comparison of 15 antipsychotic drugs in effectivity in treating schizophrenic symptoms, iloperidone demonstrated mild effectiveness. As effective as lurasidone, and 13 to 15% less effective than ziprasidone, chlorpromazine, and asenapine.[2]
It generally appears to work better than placebo.[3]
Side effects
Examination of the safety and tolerability of iloperidone have shown that at a 5 mg/day dose in healthy male volunteers, the drug was fairly well tolerated, although hypotension, dizziness, and somnolence were very common side effects ranging from mild to moderate in severity. A second study showed that co administration of food decreased the severity of these effects. This study also indicated that repeat administration of iloperidone could decrease the effects of hypotension.[4]
Iloperidone should be discontinued in patients with persistent QTc measurements of more than 500 milisecond.[5][6]
Discontinuation
The British National Formulary recommends a gradual withdrawal when discontinuing antipsychotics to avoid acute withdrawal syndrome or rapid relapse.[7] Symptoms of withdrawal commonly include nausea, vomiting, and loss of appetite.[8] Other symptoms may include restlessness, increased sweating, and trouble sleeping.[8] Less commonly there may be a feeling of the world spinning, numbness, or muscle pains.[8] Symptoms generally resolve after a short period of time.[8]
There is tentative evidence that discontinuation of antipsychotics can result in psychosis.[9] It may also result in reoccurrence of the condition that is being treated.[10] Rarely tardive dyskinesia can occur when the medication is stopped.[8]
Pharmacology
Iloperidone exerts its effects by acting upon and antagonizing specific neurotransmitters, particularly multiple dopamine and serotonin receptor subtypes. It is considered an ‘atypical’ antipsychotic because it displays serotonin receptor antagonism, similar to other atypical antipsychotics. The older typical antipsychotics are primarily dopamine antagonists.
Iloperidone has been shown to act as an antagonist at all tested receptors. It exhibits high (nM) affinity to serotonin 5HT2A (Ki value of 5.6 nM), dopamine D2 (6.3 nM) and D3 (7.1 nM) and noradrenaline α1 receptors (0.36 nM),[11] moderate affinity for dopamine D4 (25 nM), serotonin 5HT6 (43 nM), 5HT7 (22 nM), and low affinity for the serotonin 5HT1A (168 nM), dopamine D1 and histamine H1 receptors. In addition, pharmacogenomic studies identified single nucleotide polymorphisms associated with an enhanced response to iloperidone during acute treatment of schizophrenia.[3][12]
Peak plasma concentration (cMax) of iloperidone is reached 2–4 hours after oral administration.6 Its elimination half-life ranges from 18 hours for extensive cytochrome P450 (CYP2D6) metabolizers to 33 hours for poor metabolizers. The bioavailability of iloperidone is 96%. Co-administration of potent CYP2D6 or CYP3A4 inhibitors may warrant a reduction in the dose of iloperidone. It has two major metabolites: P88-8991 and P95-12113. P88-8991 shares similar receptor binding affinities with the parent compound. P95-12113 exhibits a lower affinity for the 5HT2A receptor, but does not cross the blood–brain barrier, and therefore does not contribute to the clinical effects of iloperidone.[13]
History
Hoechst Marion Roussel Inc. made initial inquiries into the drug; however, in May 1996, they discontinued research, and in June 1997 gave research rights to Titan Pharmaceuticals. Titan then handed over worldwide development, manufacturing and marketing rights to Novartis in August 1998. On June 9, 2004, Titan Pharmaceuticals announced that the Phase III development rights have been acquired by Vanda Pharmaceuticals. The original launch date was scheduled for 2002. On November 27, 2007, Vanda Pharmaceuticals announced that the U.S. Food and Drug Administration (FDA) had accepted their New Drug Application for iloperidone, confirming the application is ready for FDA review and approval.[14] On July 28, 2008, the FDA issued a not-approvable letter to Vanda Pharmaceuticals concerning the drug, stating that further trials are required before a decision can be made concerning marketed usage of iloperidone.[15]
Iloperidone was approved by the FDA for the treatment of schizophrenia in the United States on May 6, 2009.[16]
References
- Citrome, Leslie (2011-12-27). "Iloperidone: A Clinical Overview". The Journal of Clinical Psychiatry. 72 (suppl 1): 8486. doi:10.4088/JCP.10075su1.04. ISSN 0160-6689.
- Leucht S, Cipriani A, Spineli L, Mavridis D, Orey D, Richter F, Samara M, Barbui C, Engel RR, Geddes JR, Kissling W, Stapf MP, Lässig B, Salanti G, Davis JM (September 2013). "Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis". Lancet. 382 (9896): 951–62. doi:10.1016/S0140-6736(13)60733-3. PMID 23810019. S2CID 32085212.
- Scott LJ (October 2009). "Iloperidone: in schizophrenia". CNS Drugs. 23 (10): 867–80. doi:10.2165/10489070-000000000-00000. PMID 19739696.
- Sainati SM, Hubbard JW, Chi E, Grasing K, Brecher MB (July 1995). "Safety, tolerability, and effect of food on the pharmacokinetics of iloperidone (HP 873), a potential atypical antipsychotic". Journal of Clinical Pharmacology. 35 (7): 713–20. doi:10.1002/j.1552-4604.1995.tb04112.x. PMID 7560252. S2CID 24518837.
- "Fanapt (Iloperidone Tablets): Uses, Dosage, Side Effects, Interactions, Warning". RxList. Retrieved 2022-10-11.
- "Psychopharmacology Institute". psychopharmacologyinstitute.com. Retrieved 2022-10-11.
- Joint Formulary Committee, BMJ, ed. (March 2009). "4.2.1". British National Formulary (57 ed.). United Kingdom: Royal Pharmaceutical Society of Great Britain. p. 192. ISBN 978-0-85369-845-6.
Withdrawal of antipsychotic drugs after long-term therapy should always be gradual and closely monitored to avoid the risk of acute withdrawal syndromes or rapid relapse.
- Haddad P, Dursun S, Deakin B (2004). Adverse Syndromes and Psychiatric Drugs: A Clinical Guide. OUP Oxford. p. 207–216. ISBN 9780198527480.
- Moncrieff J (July 2006). "Does antipsychotic withdrawal provoke psychosis? Review of the literature on rapid onset psychosis (supersensitivity psychosis) and withdrawal-related relapse". Acta Psychiatrica Scandinavica. 114 (1): 3–13. doi:10.1111/j.1600-0447.2006.00787.x. PMID 16774655. S2CID 6267180.
- Sacchetti E, Vita A, Siracusano A, Fleischhacker W (2013). Adherence to Antipsychotics in Schizophrenia. Springer Science & Business Media. p. 85. ISBN 9788847026797.
- Mauri MC, Paletta S, Maffini M, Colasanti A, Dragogna F, Di Pace C, Altamura AC (2014-10-13). "Clinical pharmacology of atypical antipsychotics: an update". EXCLI Journal. 13: 1163–91. PMC 4464358. PMID 26417330.
- Brunton LL (2010). Goodman and Gilman's The Pharmacological Basis of Therapeutics, Twelfth Edition. New York, NY: McGraw-Hill Medical. ISBN 9780071769396.
- Rado, Jeffrey T.; Janicak, Philip G. (2014-02-26). "Long-term efficacy and safety of iloperidone: an update". Neuropsychiatric Disease and Treatment. 10: 409–415. doi:10.2147/NDT.S37824.
- "Vanda Pharmaceuticals Receives FDA Acceptance of Iloperidone New Drug Application" (Press release). Vanda Pharmaceuticals. November 27, 2007. Retrieved 2007-11-27.
- "FDA Issues Not Approvable Letter for Iloperidone to Vanda Pharmaceuticals" (Press release). Vanda Pharmaceuticals. July 28, 2008. Retrieved 2008-08-08.
- "Vanda's Schizophrenia Drug Wins Approval From U.S. Regulators" (Press release). Bloomberg. May 6, 2009. Retrieved 2009-05-06.