Vibegron
Vibegron, sold under the brand name Gemtesa, is a medication for the treatment of overactive bladder.[1][4][5]
 | |
| Clinical data | |
|---|---|
| Trade names | Gemtesa |
| Other names | KRP-114V, MK-4618 |
| AHFS/Drugs.com | |
| License data | |
| Routes of administration | By mouth |
| Drug class | Beta3 adrenergic receptor agonist |
| ATC code |
|
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Protein binding | 49.6 to 51.3% is bound to plasma proteins [2] |
| Metabolism | Predominantly oxidation and glucuronidation [2] |
| Elimination half-life | 60 to 70 hours [2] |
| Excretion | 59% feces (54% of this is in the unchanged parent drug form), 20% urine (19% of this is in the unchanged parent drug form) [3] |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.210.547 |
| Chemical and physical data | |
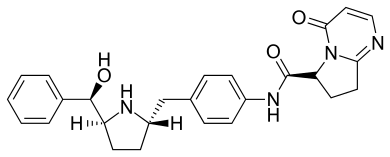
| Formula | C26H28N4O3 |
| Molar mass | 444.535 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Vibegron (other names: RVT-901; MK4618; KRP114V; URO-901) is a selective beta 3 adrenergic receptor agonist.
The most common side effects include headache, urinary tract infection, common cold, diarrhea, nausea, and upper respiratory tract infection.[4]
It was approved for medical use in the United States in December 2020.[1][4][5]
Medical uses
Vibegron is indicated for the treatment of overactive bladder with symptoms of urge urinary incontinence, urgency, and urinary frequency in adults.[1][4][5]
History and Discovery
The beta 3 adrenergic receptor was discovered in the late 1980s[6] and initially beta3AR agonists were investigated as treatment for obesity and diabetes.[7] A number of compounds were tested in clinical trials but didn't show sufficient benefits in these areas.[7]
Since the 2000s there is evidence that there are beta3AR on the detrusor muscle of the bladder.[7] The detrusor muscle contracts during urination and remains relaxed to allow the bladder to store urine.
Mirabegron was the first FDA approved selective agonist approved to treat overactive bladder (OAB).[6]
Vibegron is a selective beta3AR agonist that is developed in Japan by Kyorin Pharmaceutical Co., Ltd and Kissei Pharmaceutical Co.,Ltd and Urovant Sciences to treat overactive bladders and pain caused by irritable bowel syndrome.[8] It was globally approved on September 21, 2018, in Japan for OAB.[8]
Vibegron has been proven effective in 5 key clinical trials.[8]
A phase IIb global trial completed in 2013 of 1395 patients, of which 89.7% were women and 63.3% had not been treated previously, demonstrated a significant decrease in daily micturitions and urgent urinary incontinence episodes upon administration of vibegron.[9][10]
An international phase III trial of 506 participants completed in 2019 found statistically significant efficacy of vibegron after 2 weeks of daily administration. The adverse effect rates in patients treated with vibegron were comparable to those in patients who received a placebo.[11]
GEMTESA, a drug using vibegron as an active ingredient was approved by the FDA on December 23, 2020, after an additional phase III international trial of 1085 patients.[4]
Society and culture
Names
Vibegron is the international nonproprietary name (INN).[12]
Mechanism of action
Vibegron is a selective agonist for the beta-3 adrenergic receptor (β3-AR). The receptors are located in the kidneys, urinary tract and bladder tissue.[6] Upon binding, the β3 receptor undergoes a conformational change. This induces the activation of adenylate cyclases via G proteins and thereby promotes the formation of cyclic adenosine monophosphate (cAMP). The consequence of this cascade is an increased intracellular cAMP concentration which triggers activation of cAMP-dependent protein kinase A and causes a reduction of Ca2+ concentration in the cytoplasm. The kinase then phosphorylates myosin chains and thereby inhibits muscle contraction.[2]
The final effect of vibegron is muscle relaxation in the bladder. Due to this muscle relaxation, bladder capacity increases and symptoms of overactive bladder are relieved.[13]
Metabolism
The two main metabolic pathways are the oxidation and glucuronidation of vibegron. Two oxidative metabolites and three glucuronide metabolites can be formed. The exact structure of these metabolites have not been studied yet.[2] In vitro, CYP3A4 is the enzyme responsible for the metabolism of vibegron, facilitating oxidative metabolism. Eventually, still a large part of the unmodified drug is excreted through feces and urine.[3]
Indications
Vibegron is indicated for people with OAB. Urgency urinary incontinence (UUI), urgency and urinary frequency in adults are the most common symptoms for this condition.[3]
The drug is contraindicated in patients with known hypersensitivity to Vibegron itself or single components of the drug. The inactive components of the drug for which allergic reactions can occur are sodium croscarmellose, hydroxypropyl cellulose, magnesium stearate, mannitol and microcrystalline cellulose. The thin coating of the drug with green color contains FD&C Blue No.2.[3]
Vibegron treatment should be discontinued if urinary retention occurs. Use with nonselective muscarinic antagonists may increase the risk of urinary retention. The manufacturer suggests discontinuing vibegron if an elevated digoxin concentration occurs.[3]
Efficacy and side effects
Efficacy
Vibegron was evaluated in patients with overactive bladder (OAB) in several clinical studies. A large active-controlled study, called Empower, showed the beneficial effects of the drug to treat the condition and UUI.[3][2] Primary outcomes of different clinical trials showed there was an overall increase in efficacy. These outcomes concluded that there was a reduction in urgency to urinate, a decrease in micturitions and a decrease in average volume voided per micturition.[3] There is also an improvement observed of the symptoms when Vibegron is administered over a longer period (52 weeks) concluding that it is effective and safe for longer use.[13] In severe patients, increasing the dose was accompanied by similar beneficial effects when there was first a lack of these.[14] Quality of life of the patients is improved, including a reduction of nocturia.[13]
Adverse effects
The most common side effects of Vibegron are a dry mouth, constipation, headache, nasopharyngitis, diarrhea, nausea, bronchitis, urinary tract infection and upper respiratory tract infection. An indication is made that upon urinary retention development, the patient should stop using the drug. Risk assessment for the drug in pregnant women has yet to be evaluated.[3]
Interactions
Vibegron is in contrast to other OAB drugs very selective and leads to a lesser degree in unwanted side effects. Vibegron is found to be a substrate for CYP3A4 in vivo, but does not actually induce or inhibit any of the cytochrome P450 enzymes and is thus less likely to take part in drug–drug interactions (DDI). Here vibegron differs from the previous overactive bladder drug mirabegron, which was known to be associated in various drug–drug interactions by inhibiting CYP2D6 or inducing CYP3A4, CYP2D6 and CYP2C9 in the liver.[10][2][15][16][17][13]
Using Vibegron only (monotherapy) has positive effects on OAB and UUI, but a combination with other drugs can have additional effects. In a study with antimuscarinic drugs, more DDIs were investigated using a model of Rhesus monkeys. Dose combinations of vibegron and tolterodine showed increased bladder capacity, the effects of both drugs at low dosis strengthened each other, known as synergism. The addition of darifenacin to vibegron created greater bladder relaxation only when used at high doses.[18] Additionally, co-administration with Imidafenacin shows an increase in bladder capacity and voided volume in comparison to monotherapy.[18] Possibly, a widely adapted treatment will be the combination of beta-3-adrenergic agonist with a nonselective M2/M3 antagonist as the most prevalent option.[2]
Clinical studies show no significant drug–drug interaction (DDI), aside from a serum concentration increase of digoxin when taken with vibegron. Maximal concentrations and systemic exposure (Cmax and area under the curve (AUC)) of digoxin are both increased as a result of DDI.[19][3] Apart from the no to little DDIs, Vibegron has an additional safety quality in that it does not cross the blood-brain barrier and therefore does not induce cognitive impairment.[2] Furthermore, Vibegron can be taken with or without food, this does not have an effect on vibegron plasma concentrations.[3][19]
Toxicity
Effects on animals
Pregnant rats were given very high daily oral doses of Vibegron during the period of organogenesis and showed no embryo-fetal developmental toxicity up to 300 mg/kg/day. Similar data was found in rabbits. Maternal toxicity was observed when doses exceeded 100 mg/kg/day in lactating rats. Clinical studies show that Vibegron is not toxic, safe and well-tolerated in patients.[3]
References
- "Gemtesa- vibegron tablet, film coated". DailyMed. Retrieved 12 January 2021.
- Rechberger T, Wróbel A (January 2021). "Evaluating vibegron for the treatment of overactive bladder". Expert Opinion on Pharmacotherapy. 22 (1): 9–17. doi:10.1080/14656566.2020.1809652. ISSN 1465-6566. PMID 32993398. S2CID 222166213.
- Urovant Sciences GmbH (2020). "HIGHLIGHTS OF PRESCRIBING INFORMATION GEMTESA" (PDF).
{{cite web}}: CS1 maint: url-status (link) - "Drug Trials Snapshot: Gemtesa". U.S. Food and Drug Administration (FDA). 23 December 2020. Retrieved 12 January 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "Sumitovant Biopharma Announces Urovant Sciences Receives U.S. FDA Approval of Gemtesa (vibegron) 75 mg Tablets for the Treatment of Patients with Overactive Bladder (OAB)" (Press release). Sumitovant Biopharma. 23 December 2020. Retrieved 23 December 2020 – via GlobeNewswire.
- Schena G, Caplan MJ (April 2019). "Everything You Always Wanted to Know about β3-AR * (* But Were Afraid to Ask)". Cells. 8 (4): 357. doi:10.3390/cells8040357. PMC 6523418. PMID 30995798.
- Edmondson SD, Zhu C, Kar NF, Di Salvo J, Nagabukuro H, Sacre-Salem B, et al. (January 2016). "Discovery of Vibegron: A Potent and Selective β3 Adrenergic Receptor Agonist for the Treatment of Overactive Bladder". Journal of Medicinal Chemistry. 59 (2): 609–23. doi:10.1021/acs.jmedchem.5b01372. PMID 26709102.
- Keam SJ (November 2018). "Vibegron: First Global Approval". Drugs. 78 (17): 1835–1839. doi:10.1007/s40265-018-1006-3. PMID 30411311. S2CID 53212220.
- Merck Sharp & Dohme Corp. (15 March 2011). "A Study of the Efficacy and Safety of Vibegron (MK-4618) in Participants With Overactive Bladder (OAB) (MK-4618-008)".
{{cite web}}: CS1 maint: url-status (link) - Mitcheson HD, Samanta S, Muldowney K, Pinto CA, Rocha BA, Green S, et al. (February 2019). "Vibegron (RVT-901/MK-4618/KRP-114V) Administered Once Daily as Monotherapy or Concomitantly with Tolterodine in Patients with an Overactive Bladder: A Multicenter, Phase IIb, Randomized, Double-blind, Controlled Trial". European Urology. 75 (2): 274–282. doi:10.1016/j.eururo.2018.10.006. PMID 30661513.
- Urovant Sciences GmbH (11 July 2018). "An Extension Study to Examine the Safety and Tolerability of a New Drug in Patients With Symptoms of Overactive Bladder (OAB). (Empowur)".
{{cite journal}}: Cite journal requires|journal=(help)CS1 maint: url-status (link) - World Health Organization (2013). "International nonproprietary names for pharmaceutical substances (INN): recommended INN: list 70". WHO Drug Information. 27 (3): 318. hdl:10665/331167.
- Yoshida M, Takeda M, Gotoh M, Yokoyama O, Kakizaki H, Takahashi S, et al. (March 2019). "Efficacy of novel β3 -adrenoreceptor agonist vibegron on nocturia in patients with overactive bladder: A post-hoc analysis of a randomized, double-blind, placebo-controlled phase 3 study". International Journal of Urology. 26 (3): 369–375. doi:10.1111/iju.13877. PMC 6912249. PMID 30557916.
- Yoshida M, Takeda M, Gotoh M, Nagai S, Kurose T (May 2018). "Vibegron, a Novel Potent and Selective β3-Adrenoreceptor Agonist, for the Treatment of Patients with Overactive Bladder: A Randomized, Double-blind, Placebo-controlled Phase 3 Study". European Urology. 73 (5): 783–790. doi:10.1016/j.eururo.2017.12.022. PMID 29366513.
- Stambakio H (2019). "AUA 2019: Once-Daily Vibegron, a Novel Oral β3 Agonist Does Not Inhibit CYP2D6, a Common Pathway For Drug Metabolism in Patients on OAB Medications".
{{cite web}}: CS1 maint: url-status (link) - Bragg R, Hebel D, Vouri SM, Pitlick JM (December 2014). "Mirabegron: a Beta-3 agonist for overactive bladder". The Consultant Pharmacist. 29 (12): 823–37. doi:10.4140/TCP.n.2014.823. PMC 4605389. PMID 25521658.
- Araklitis G, Baines G, da Silva AS, Robinson D, Cardozo L (11 September 2020). "Recent advances in managing overactive bladder". F1000Research. 9: 1125. doi:10.12688/f1000research.26607.1. PMC 7489273. PMID 32968482.
- Di Salvo J, Nagabukuro H, Wickham LA, Abbadie C, DeMartino JA, Fitzmaurice A, et al. (February 2017). "Pharmacological Characterization of a Novel Beta 3 Adrenergic Agonist, Vibegron: Evaluation of Antimuscarinic Receptor Selectivity for Combination Therapy for Overactive Bladder". The Journal of Pharmacology and Experimental Therapeutics. 360 (2): 346–355. doi:10.1124/jpet.116.237313. PMID 27965369.
- Medscape. "vibegron (Rx)".
{{cite web}}: CS1 maint: url-status (link)
External links
- "Vibegron". Drug Information Portal. U.S. National Library of Medicine.
- Clinical trial number NCT03492281 for "A Study to Examine the Safety and Efficacy of a New Drug in Patients With Symptoms of Overactive Bladder (OAB) (Empowur)" at ClinicalTrials.gov