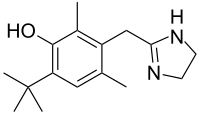
Oxymetazoline
Oxymetazoline, sold under the brand name Afrin among others, is a topical decongestant and vasoconstrictor medication. It is available over-the-counter as a nasal spray to treat nasal congestion and nosebleeds, as eyedrops to treat eye redness due to minor irritation, and (in the United States) as a prescription topical cream to treat persistent facial redness due to rosacea in adults. Its effects begin within minutes and last for up to 6 hours. Intranasal use for longer than three days may cause congestion to recur or worsen, resulting in physical dependence.
 | |
| Clinical data | |
|---|---|
| Trade names | Afrin, Ocuclear, Drixine, Rhofade |
| AHFS/Drugs.com | Monograph |
| Pregnancy category |
|
| Dependence liability | Moderate |
| Routes of administration | Intranasal, Eye drop |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Metabolism | Kidney (30%), fecal (10%) |
| Elimination half-life | 5–6 hours |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.014.618 |
| Chemical and physical data | |
| Formula | C16H24N2O |
| Molar mass | 260.381 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 301.5 °C (574.7 °F) |
SMILES
| |
InChI
| |
| | |
Oxymetazoline is a derivative of imidazole.[1] It was developed from xylometazoline at E. Merck Darmstadt by Wolfgang Fruhstorfer and Helmut Müller-Calgan in 1961.[2] A direct sympathomimetic, oxymetazoline binds to and activates α1 adrenergic receptors and α2 adrenergic receptors, most notably.[1] One study classified it in the following order: α(2A) > α(1A) ≥ α(2B) > α(1D) ≥ α(2C) >> α(1B), but this is not universally agreed upon.[3] There is little consistency across the (relatively large) number of in-vitro studies with respect to binding affinity/selectivity.
Medical uses
Oxymetazoline is available over-the-counter as a topical decongestant in the form of oxymetazoline hydrochloride in nasal sprays such as Otrivin, Afrin, Operil, Dristan, Dimetapp, Oxyspray, Facimin, Nasivin, Nostrilla, Utabon, Sudafed OM, Vicks Sinex, Zicam, SinuFrin, Drixoral[4] and Mucinex Full Force.[5]
In the United States, oxymetazoline 1% cream is approved by the Food and Drug Administration for topical treatment of persistent facial erythema (redness) associated with rosacea in adults.[6]
Due to its vasoconstricting properties, oxymetazoline is also used to treat nose bleeds[7][8] and eye redness due to minor irritation (marketed as Visine L.R. in the form of eye drops). [9]
In July 2020, oxymetazoline received approval by the FDA for the treatment of acquired drooping eyelid.[10]
Side effects
Rebound congestion
Rebound congestion, or rhinitis medicamentosa, may occur. A 2006 review of the pathology of rhinitis medicamentosa concluded that use of oxymetazoline for more than three days may result in rhinitis medicamentosa and recommended limiting use to three days.[11]
Australian regulatory submission
In a submission to the Therapeutic Goods Administration, a Novartis representative concluded, "The justification was not based on evidence." Citing an existing extensive body of evidence and noting a range of recommended periods from five to ten days, Novartis recommended the established five day period for its use for self-medication without medical consultation as it coincides with the typical duration of the common cold.[12]
Use in pregnancy
The Food and Drug Administration places oxymetazoline in category C, indicating risk to the fetus cannot be ruled out. While it has been shown that a single dose does not significantly alter either maternal or fetal circulation,[13] this subject has not been studied extensively enough to draw reliable conclusions.
Overdose
If accidentally ingested, standard methods to remove unabsorbed drugs should be considered. There is no specific antidote for oxymetazoline, although its pharmacological effects may be reversed by an adrenergic antagonists such as phentolamine. In the event of a possibly life-threatening overdose (such as a hypertensive crisis), benzodiazepines should be considered to decrease the likelihood of seizures and convulsions, as well as reduce anxiety and to lower blood pressure. In children, oxymetazoline may produce profound central nervous system depression due to stimulation of central α2 receptors and imidazoline receptors, much like clonidine.
Pharmacology
Pharmacodynamics
Oxymetazoline is a sympathomimetic that selectively agonizes α1 and, partially, α2 adrenergic receptors.[14] Since vascular beds widely express α1 receptors, the action of oxymetazoline results in vasoconstriction. In addition, the local application of the drug also results in vasoconstriction due to its action on endothelial postsynaptic α2 receptors; systemic application of α2 agonists, in contrast, causes vasodilation because of centrally-mediated inhibition of sympathetic tone via presynaptic α2 receptors.[15] Vasoconstriction of vessels results in relief of nasal congestion in two ways: first, it increases the diameter of the airway lumen; second, it reduces fluid exudation from postcapillary venules.[16] It can reduce nasal airway resistance (NAR) up to 35.7% and reduce nasal mucosal blood flow up to 50%.[17]
Pharmacokinetics
Since imidazolines are sympathomimetic agents, their primary effects appear on α adrenergic receptors, with little if any effect on β adrenergic receptors.[18] Like other imidazolines, Oxymetazoline is readily absorbed orally.[18] Effects on α receptors from systemically absorbed oxymetazoline hydrochloride may persist for up to 7 hours after a single dose. The elimination half-life in humans is 5–8 hours.[19] It is excreted unchanged both by the kidneys (30%) and in feces (10%).
History
The oxymetazoline brand Afrin was first sold as a prescription medication in 1966. After finding substantial early success as a prescription medication, it became available as an over-the-counter drug in 1975. Schering-Plough did not engage in heavy advertising until 1986.[20]
From the mid-1980s to mid-1990s, the brand Sinex was featured in many television advertisements. Some of these commercials showed men, women, and children using other brands of nasal sprays, and then standing upside down on a sidewalk, or against a wall, etc. or hanging upside down from various playground equipment to prevent their nasal spray from dripping out. This was juxtaposed with Sinex users not having to hang upside side down or stand on their heads as it didn't drip out.
Brand names
Brand names include Afrin, Drixine, Dristan, Nasivin, Nasivion, Nezeril, Nostrilla, Logicin, Vicks Sinex, Visine L.R., Sudafed OM, Zicam, Otrivin Oxy, SinuFrin, Upneeq, and Mucinex Sinus-Max.
References
- PubChem [Internet]. Bethesda (MD): National Library of Medicine (US), National Center for Biotechnology Information; 2004-. PubChem Compound Summary for CID 4636, Oxymetazoline; [cited 2021 Apr. 18]. Available from: https://pubchem.ncbi.nlm.nih.gov/compound/Oxymetazoline
- German Patent 1,117,588
- Haenisch, Britta; Walstab, Jutta; Herberhold, Stephan; Bootz, Friedrich; Tschaikin, Marion; Ramseger, René; Bönisch, Heinz (December 2010). "Alpha-adrenoceptor agonistic activity of oxymetazoline and xylometazoline". Fundamental & Clinical Pharmacology. 24 (6): 729–739. doi:10.1111/j.1472-8206.2009.00805.x. ISSN 1472-8206. PMID 20030735. S2CID 25064699.
- "Drixoral Decongestant Nasal Spray". Bayer. Retrieved 18 November 2017.
- "Oxymetazoline: Drug Information Provided by Lexi-Comp: Merck Manual Professional". Merck.com. Retrieved 15 April 2013.
- Patel NU, Shukla S, Zaki J, Feldman SR (October 2017). "Oxymetazoline hydrochloride cream for facial erythema associated with rosacea". Expert Review of Clinical Pharmacology. 10 (10): 1049–1054. doi:10.1080/17512433.2017.1370370. PMID 28837365. S2CID 19930755.
- Katz RI, Hovagim AR, Finkelstein HS, Grinberg Y, Boccio RV, Poppers PJ (1990). "A comparison of cocaine, lidocaine with epinephrine, and oxymetazoline for prevention of epistaxis on nasotracheal intubation". Journal of Clinical Anesthesia. 2 (1): 16–20. doi:10.1016/0952-8180(90)90043-3. PMID 2310576.
- Krempl GA, Noorily AD (September 1995). "Use of oxymetazoline in the management of epistaxis". The Annals of Otology, Rhinology, and Laryngology. 104 (9 Pt 1): 704–6. doi:10.1177/000348949510400906. PMID 7661519. S2CID 37579139.
- "VISINE® Original Red Eye Drops | VISINE products". Visine.com. Archived from the original on 2 December 2010. Retrieved 15 April 2013.
- "UPNEEQ® Label" (PDF). accessdata.fda.gov. 8 July 2020.
- Ramey JT, Bailen E, Lockey RF (2006). "Rhinitis medicamentosa". Journal of Investigational Allergology & Clinical Immunology. 16 (3): 148–55. PMID 16784007.
- Nguyen, Tra-My (2014). "Consultation submission: OTC nasal decongestant preparations for topical use: proposed advisory statements for medicines" (PDF). Novartis Consumer Health Australasia.
- Rayburn WF, Anderson JC, Smith CV, Appel LL, Davis SA (August 1990). "Uterine and fetal Doppler flow changes from a single dose of a long-acting intranasal decongestant". Obstetrics and Gynecology. 76 (2): 180–2. PMID 2196495.
- Westfall Thomas C, Westfall David P, "Chapter 6. Neurotransmission: The Autonomic and Somatic Motor Nervous Systems" (Chapter). Brunton LL, Lazo JS, Parker KL: Goodman & Gilman's The Pharmacological Basis of Therapeutics, 11e: "AccessMedicine | Anatomy and General Functions of the Autonomic and Somatic Motor Nervous Systems". Archived from the original on 30 September 2011. Retrieved 24 January 2015..
- Biaggioni I, Robertson D. "Chapter 9. Adrenoceptor Agonists & Sympathomimetic Drugs". In Katzung BG (ed.). Basic & Clinical Pharmacology (11th ed.). Archived from the original on 30 September 2011. Retrieved 30 November 2011.
- Widdicombe J (1997). "Microvascular anatomy of the nose". Allergy. 52 (40 Suppl): 7–11. doi:10.1111/j.1398-9995.1997.tb04877.x. PMID 9353554. S2CID 46018611.
- Bende M, Löth S (March 1986). "Vascular effects of topical oxymetazoline on human nasal mucosa". The Journal of Laryngology and Otology. 100 (3): 285–8. doi:10.1017/S0022215100099151. PMID 3950497. S2CID 37998936.
- Clinical veterinary toxicology. Konnie H. Plumlee. St. Louis, Mo.: Mosby. 2004. ISBN 978-0-323-01125-9. OCLC 460904351.
{{cite book}}: CS1 maint: others (link) - Dalefield, Rosalind (2017). Veterinary toxicology for Australia and New Zealand. Amsterdam, Netherlands. ISBN 978-0-12-799912-8. OCLC 992119220.
- Dougherty, Phillip H. (20 October 1986). "Advertising; Afrin Goes After Users Of Nasal Decongestants". The New York Times. Retrieved 30 March 2015.