Desonide
 | |
| Names | |
|---|---|
| Trade names | Desonate, DesOwen, Verdeso, others[1] |
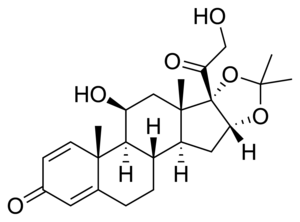
| Other names | Prednacinolone; Hydroxyprednisolone acetonide; Desfluorotriamcinolone acetonide; (11β,16α)-11,21-Dihydroxy-16,17-[(1-methylethylidene)bis(oxy)]-pregna-1,4-diene-3,20-dione |
IUPAC name
| |
| Clinical data | |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Pregnancy category |
|
| Routes of use | Topical |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a605025 |
| Legal | |
| Legal status |
|
| Chemical and physical data | |
| Formula | C24H32O6 |
| Molar mass | 416.514 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Desonide is a steroid cream used to treat eczema, seborrheic dermatitis, contact dermatitis, and psoriasis.[1] It comes as a cream, ointment, lotion, and foam.[1]
Common side effects include burning, folliculitis, acne, and thinning of the skin.[1] Other side effects may include Cushing’s syndrome and high blood sugar.[1] Most side effects are mild.[2] It has low to mid potency and is classified as a group VI corticosteroid in the USA.[1][3]
Desonide was approved for medical use in the United States in 1972.[1] It is available as a generic medication under various brandnames.[4][1] A 15 gram tube of 0.05% costs about 15 USD as of 2021.[4]
Medical uses
Desonide is a prescription topical treatment for redness, swelling, itching, and discomfort of various skin conditions. Regardless of the vehicle used, desonide is applied 2 to 3 times a day, at the same times each day. Skin conditions typically improve in the first two weeks of treatment. People are instructed to use desonide for the minimum amount of time necessary for conditions to improve.[5]
Side effects
The safety of desonide has not been determined beyond 4 weeks of use.[5] People with allergies to corticosteroids (like hydrocortisone or prednisone) should use caution when taking desonide.[6] Pharmacists and prescribing physicians should be aware that this medication may contain inactive ingredients than can cause allergic reactions.
Desonide should not be used if there is an infection or open wound in the treatment area.
Systemic absorption of topical corticosteroids can produce adverse effects. Indication of Cushing's syndrome, hyperglycemia, and glycosuria have been observed in some patients receiving treatment. After stopping treatment, reversible hypothalamic-pituitary-adrenal (HPA) axis suppression with the potential for glucocorticosteroid insufficiency is possible. The cosyntropin (ACTH1-24) laboratory test can evaluate patients for HPA axis suppression.[5] HPA function can be reversed after the cessation of treatment or replacement with another less potent corticosteroid. If glucocorticosteroid insufficiency occurs, supplemental systemic corticosteroids may be required.
Side effects of desonide requiring immediate contact with the prescribing physician:
- Blistering, burning, crusting, dryness, or flaking of the skin
- burning, itching, redness, skin rash, swelling, or soreness at the application site
- flushing or redness of the skin
- irritation
- itching, scaling, severe redness, soreness, or swelling of the skin
- peeling of the skin
- raised, dark red, wart-like spots on the skin, especially when used on the face
- stinging and burning
- unusually warm skin
Side effects that may go away as the body adjusts to the medication:
- Body aches or pain
- chills
- cough
- difficulty with breathing
- ear congestion
- fever
- headache
- loss of voice
- nasal congestion
- runny nose
- sneezing
- sore throat
- unusual tiredness or weakness
Pregnancy
The FDA has labeled desonide as pregnancy category C. Desonide should only be used during pregnancy when absolutely necessary.
Breastfeeding
It is currently unknown whether topical application of Desonide can pass into breast milk. Similar drugs taken orally have been seen to pass into breast milk. The prescribing doctor should be consulted prior to breast-feeding.
Interactions
Common medications causing a minor negative drug interaction include: Insulin and Metformin. Common medications checked in combination, but that are not known to create a negative drug interaction, include: Aspirin, Cymbalta (duloxetine), Fish Oil, Acetaminophen, Vitamin B12, Vitamin C, Vitamin D3, and Zyrtec.[7]
Mechanism of action
Desonide is a synthetic nonfluorinated corticosteroid; topical corticosteroids have anti-inflammatory, antipruritic, and vasoconstrictive properties. The mechanism of these properties, however, is unclear for the dermal route of administration.[8] Following absorption through the skin, corticosteroids follow pharmacokinetic pathways similarly to intravenously administered corticosteroids. The mechanism of corticosteroids is thought to induce phospholipase A2 inhibitory proteins (lipocortins). Lipocortins control the biosynthesis of inflammation mediators, like prostaglandins and leukotrienes. Lipocortins can inhibit the common precursor of inflammation mediators, arachidonic acid.
History
Desonide was first introduced in the United States under the trade name Tridesilon by Dome Laboratories in 1970.[9] Since the discovery in the United States, several other countries have introduced different brand names of desonide, including Italy, Spain, United Kingdom, and Germany. The FDA first approved Connetics Corporation’s Verdeso Foam® on September 16, 2006.[10] Just shortly after, the FDA approved SkinMedica Inc.’s Desonate® hydrogel delivery vehicle on October 20, 2006.[11]
Society and culture
Cost
The cost in the U.S. for topical ointment 0.05% for 15 grams is $26 (USD)[12]
.svg.png.webp) Desonide costs (US)
Desonide costs (US).svg.png.webp) Desonide prescriptions (US)
Desonide prescriptions (US)
Regulatory
The first US. patent for desonide was US4185100A was granted on January 22, 1980.[13] The patent was for topical anti-inflammatory treatment using desonide. The patent defends the suitability of the anti-inflammatory for the treatment of cutaneous disorders or disruptions characterized by skin inflammation and/or hyperproliferative activity in the epidermis. Side effects and the mechanism of action are both disclosed. This patent is currently expired.
Research
Desonate was approved by the FDA following two major clinical trials in 2006. Each randomized, double-blind, placebo-controlled study enrolled 582 pediatric patients (between the ages of 3 months and 18 years).[14] The patient was topically administered the drug or placebo two times a day for four weeks. Using the Investigator’s Global Severity Score (IGSS), the treatment was considered successful if at Week 4 there was at least a two (2) point decrease from the patient’s baseline IGSS. In clinical trial 1, 44% of patients succeeded successful treatment of Desonate versus 14% treated with the placebo. In clinical trial 2, 28% of patients succeeded successful treatment of Desonate versus 6% treated with the placebo.
The FDA approved Tridesilon for the following treatments: Contact Dermatitis, Rhus Dermatitis, Eczema, Dermatitis, Discoid Lupus Erythematosus, Granuloma Annulare, Seborrheic Dermatitis, Polymorphous Light Eruption, Pruritus, Psoriasis, Lichen Simplex, Atopic Dermatitis, Lichen Planus, Xerosis, Exfoliative Dermatitis.[15]
Recently, in late 2014, phase 3 clinical trials were completed to evaluate treatments using Desonide cream versus amino acid moisturizing cream.[16] Patients with eczema or atopic dermatitis could be enrolled in this study, both male and female, over the age of 18. The randomized, double-blind, active control, 5-week study compared the effects of treatment of both creams through twice-a-day application. The clinical trial is sponsored by NeoStrata Company, Inc.
No research has been completed to evaluate the carcinogenic or photoco-carcinogenic potential of desonide. Additionally, no research has been completed to determine the effect on fertility.[5] These are current opportunities for improvement to learn more about the risks and benefits associated with desonide.
References
- 1 2 3 4 5 6 7 8 "Desonide Monograph for Professionals". Drugs.com. Archived from the original on 20 September 2020. Retrieved 17 July 2021.
- ↑ Wong VK, Fuchs B, Lebwohl M (2004). "Overview on desonide 0.05%: a clinical safety profile". Journal of Drugs in Dermatology. 3 (4): 393–7. PMID 15303783.
- ↑ Bope, Edward T.; Kellerman, Rick D. (24 November 2015). Conn's Current Therapy 2016. Elsevier Health Sciences. p. PT262. ISBN 978-0-323-35535-3. Archived from the original on 28 August 2021. Retrieved 17 July 2021.
- 1 2 "Desonide Prices, Coupons & Savings Tips - GoodRx". GoodRx. Archived from the original on 23 June 2019. Retrieved 17 July 2021.
- 1 2 3 4 "Access Data FDA" (PDF). FDA.gov. Archived (PDF) from the original on February 25, 2017. Retrieved December 1, 2015.
- ↑ "desonide topical : Uses, Side Effects, Interactions, Pictures, Warnings & Dosing - WebMD". WebMD. Archived from the original on 2015-11-26. Retrieved 2015-11-30.
- ↑ "Desonide topical Drug Interactions - Drugs.com". Drugs.com. Archived from the original on 2018-07-12. Retrieved 2018-07-12.
- ↑ "Desonate (desonide) - Drug information from MediLexicon". www.medilexicon.com. Archived from the original on 2015-12-08. Retrieved 2015-11-30.
- ↑ Sittig M (1988). "Pharmaceutical Manufacturing Encyclopedia" (PDF). Noyes Publications. Archived from the original (PDF) on October 23, 2007. Retrieved December 1, 2015.
- ↑ "Verdeso (desonide) FDA Approval History - Drugs.com". www.drugs.com. Archived from the original on 2015-12-08. Retrieved 2015-12-01.
- ↑ "Desonate (desonide) FDA Approval History - Drugs.com". www.drugs.com. Archived from the original on 2015-12-08. Retrieved 2015-12-01.
- ↑ "Desonide topical Prices, Coupons & Patient Assistance Programs". Drugs.com. Archived from the original on 20 September 2020. Retrieved 27 March 2021.
- ↑ US 4185100, Rovee DT, Marvel JR, Mezick JA, "Topical anti-inflammatory drug therapy", issued 22 January 1980, assigned to Johnson and Johnson
- ↑ Jorizzo J, Levy M, Lucky A, Shavin J, Goldberg G, Dunlap F, et al. (July 1995). "Multicenter trial for long-term safety and efficacy comparison of 0.05% desonide and 1% hydrocortisone ointments in the treatment of atopic dermatitis in pediatric patients". Journal of the American Academy of Dermatology. 33 (1): 74–7. doi:10.1016/0190-9622(95)90014-4. PMID 7601950.
- ↑ "Tridesilon Topical Cream 0.05pct Drug Medication Dosage Information". www.cvs.com. Archived from the original on 2015-12-08. Retrieved 2015-12-01.
- ↑ Clinical trial number NCT02286700 for "A clinical trial to evaluate treatments using Desonide Cream and Amino Acid Moisturizing Cream for patients with Eczema or Atopic Dermatitis" at ClinicalTrials.gov
External links
| Identifiers: |
|---|