Mpox
| Mpox | |
|---|---|
| Other names: Monkeypox | |
 | |
| Various appearances of mpox spots | |
| Specialty | Infectious disease[1] |
| Symptoms | None, fever, headache, muscle pains, swollen lymph nodes, blistering rash[2][3] |
| Complications | Secondary infections, eye infection, vision loss, scarring[3][4] |
| Usual onset | 5 to 21 days post exposure[3] |
| Duration | 2 to 4 weeks[5] |
| Types | Central African (Congo Basin), West African[6] |
| Causes | Monkeypox virus[4] |
| Risk factors | Hunters in Central and West Africa[7] |
| Diagnostic method | Testing for viral DNA (PCR)[8] |
| Differential diagnosis | Chickenpox, shingles, measles, syphilis, smallpox, scabies, bacterial skin infection, drug eruption[3] |
| Prevention | Smallpox vaccines, hand washing, covering rash, PPE, keep away from sick people[9][10] |
| Treatment | Supportive, antivirals, vaccinia immune globulin[11] |
| Medication | Cidofovir, tecovirimat[3] |
| Prognosis | Most recover[12] |
| Frequency | Not as rare as previously thought[13] |
| Deaths | <1%: West African type[14] Up to 11%: Central African type[3] |
Mpox, previously known as monkeypox, is an infectious viral disease that can occur in both humans and some other animals.[1] Symptoms include fever, swollen lymph nodes, and a rash that forms blisters and than crusts over.[15] The time from exposure to onset of symptoms ranges from 5-to-21 days.[3] The duration of symptoms is typically 2 to 4 weeks.[5] There may be mild symptoms, but to what extent it may occur without symptoms is not known.[3][16] The classic presentation of fever and muscle pains, followed by swollen glands, with lesions all at the same stage, has not been found to be common in all outbreaks.[15][17] The skin lesions can number from none to many, occur before glands swell, and can appear in one area at different stages of development.[18]
The disease is caused by monkeypox viruses, a type of Orthopoxvirus.[4] Of the 2-types in humans, the West African type causes a less severe disease than the Central African (Congo Basin) type.[19] It may spread from handling bushmeat, animal bites or scratches, body fluids, contaminated objects, or other close contact with an infected person.[20][21] Spread can occur by small droplets and possibly the airborne route.[10][15][22] People can spread the virus from the onset of symptoms until all the lesions have scabbed and fallen off; with some evidence of spread for more than a week after lesions have crusted.[19] The virus is believed to normally spread among certain rodents in Africa.[20] Diagnosis can be confirmed by testing a lesion for the virus's DNA.[8] It can appear similar to chickenpox, measles and smallpox, but may be distinguished by the presence of swollen glands.[3][23]
There is no known cure.[24] The smallpox vaccine was found to be around 85% protective in preventing infection in close contacts and in lessening the severity of the disease.[4] A newer MVA-BN smallpox vaccine has been approved, but with limited availability.[3][9] Other measures include regular hand washing and avoiding sick people and other animals.[25] The antiviral medication cidofovir and tecovirimat, vaccinia immune globulin, and the smallpox vaccine may be used during outbreaks.[11][12] The risk of death has varied from 0% to 11%.[3] Most people recover.[12] The disease is more severe in the very young, malnourished people, pregnant women, and in those with weakened immune systems.[26]
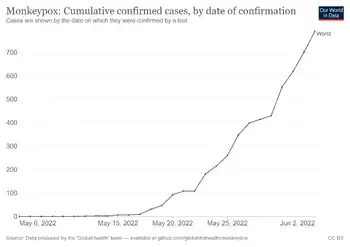
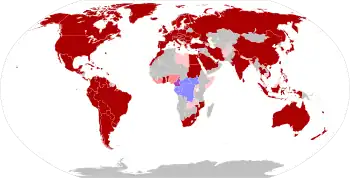
The disease is no longer believed to be as rare as previously thought;[13][27] possibly as a result of waning immunity since the stopping of routine smallpox vaccination.[23] Cases have significantly increased since the 1980s.[28] Sporadic cases occur in Central and West Africa, and it is common in the Democratic Republic of Congo (DRC).[27] Hunters in the tropical forests of Central and West Africa are most at risk.[7] It was first identified as a distinct illness in 1958 among laboratory monkeys in Denmark.[29][30] The first case in humans was reported in 1970 in the DRC, during smallpox eradication efforts.[31] The first cases in humans outside of Africa presented in the United States in 2003, when the outbreak was traced to a pet store where imported rodents were sold.[8] Since 2017, a large outbreak has been occurring in Nigeria.[32] Since mid-May 2022, cases have been reported with spread between people, in several countries that do not typically see the disease, including countries in Europe, North America, South America and Australasia.[15] On 23 July 2022, the World Health Organization (WHO) declared the 2022 monkeypox outbreak a Public Health Emergency of International Concern.[33] This was withdrawn in May of 2023.[34] Due to stigma associated with the term "monkeypox", the WHO renamed the disease mpox in November 2022.[35]
Signs and symptoms
The disease may be suspected by its classical signs and symptoms that follow a sequential course of an early stage followed by a rash.[36] There may be mild symptoms, but to what extent it may occur without symptoms is not known.[3] Sometimes there is a sore throat and cough.[2] A person is not believed to be contagious during the incubation period.[2] The illness appears to vary between different outbreaks.[17] Initial features in the 2003 outbreak were typically skin lesions or high fever with intense sweating and chills.[37] Other frequently seen symptoms included cough, sore throat, and some had diarrhea, nasal congestion, nausea and blepharitis.[37] Symptoms may vary in people with HIV.[16] Many cases in the 2022 monkeypox outbreak presented with genital and peri-anal lesions, fever, swollen lymph nodes, and pain when swallowing.[15]
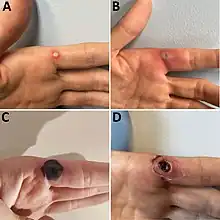 Progression of monkeypox after needlestick injury from a pustule at work[38]
Progression of monkeypox after needlestick injury from a pustule at work[38]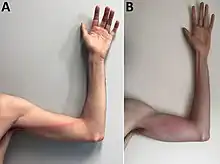 Tender, indurated, erythematous, and well-delimited linear streak from the left finger to the armpit, on the seventh day of illness. B) Aggravated lymphangitis on the ninth day of illness.
Tender, indurated, erythematous, and well-delimited linear streak from the left finger to the armpit, on the seventh day of illness. B) Aggravated lymphangitis on the ninth day of illness. Mpox lesions on a penis
Mpox lesions on a penis
Initial

The time from exposure to onset of symptoms is on average 12 days;[4] though ranges from 5-to-21 days.[3] Early symptoms include fever, headache, shivering, muscle pains, backache and feeling extremely tired.[39] It may initially appear like flu.[26] Large painful swollen glands, typically behind the ear, below the jaw, in the underarms, in the neck or in the groin, occur before the onset of the rash.[2] The swollen glands may be localised or generalised, and be on both sides of the body or just one.[2] Transmission of infection during this phase may be possible.[40]
Rash
The disease can initially appear similar to chickenpox, measles and smallpox, but distinguished by the presence of the swollen glands.[3] Within a few days of the fever, lesions characteristically appear in the mouth and on the face before appearing elsewhere such as hands and feet.[41] Three-quarters of affected people have the bumps on the palms and soles, more than two-thirds in the mouth, around a third on the genitals and one in five have lesions in the eyes.[3] They begin as small flat spots, before becoming small bumps which then fill with at first clear fluid and then yellow fluid, which subsequently burst and scab over before falling off.[3] In each part of the body affected, the spots usually evolve in the same stage.[42] There may be a few bumps or several thousand, sometimes merging to produce large lesions.[3] Each ranges from around 0.5cm to 1cm and may have a central dip.[40][10] The lesions may be either itchy or painful.[14]
The rash typically lasts around 10-days.[26] An affected person may remain unwell for 2-to-4 weeks.[5]
 Mpox forehead
Mpox forehead Mpox - palms (1997)
Mpox - palms (1997) Mpox
Mpox Mpox
Mpox
Complications
Complications include secondary infections, pneumonia, sepsis and encephalitis.[3] Infection in the eye may lead to corneal damage and loss of vision.[40]
If infection occurs during pregnancy still birth or birth defects may occur.[14] The disease may be milder in people vaccinated against smallpox in childhood.[12]
Cause
Mpox is a zoonotic poxvirus infection that can occur in both humans and some other animals.[4] Two recognized distinct types are described as the Congo Basin clade and the milder West African clade.[4]
Virology
Mpox is caused by the monkeypox virus, a type of Orthopoxvirus, a genus of the family Poxviridae that contains other viral species that target mammals.[4] Two groups have been characterised; Central African and West African.[6] The West African type generally results in milder disease than the Central African type.[14]
The natural host reservoir is unknown, but may be more than one.[6] The virus has been found in the African striped squirrel in 1985 in the DRC, and the sooty mangabey in 2012 in Cote d’Ivoire.[43] In addition to monkeys, reservoirs for the virus are found in Gambian pouched rats (Cricetomys gambianus), dormice (Graphiurus spp.) and African squirrels (Heliosciurus, and Funisciurus).[44] The use of these animals as food may be an important source of transmission to humans.[44]
 Scanning electron micrograph of mpox virus orange on the surface of infected VERO E6 cells
Scanning electron micrograph of mpox virus orange on the surface of infected VERO E6 cells.jpg.webp) Colorized transmission electron micrograph of mpox virus particles (green)
Colorized transmission electron micrograph of mpox virus particles (green)
Spread
Humans can be infected by an animal via a bite, or by direct contact with an infected animal’s bodily fluids.[45][46] The virus can also be transmitted from one person to another by close contact with a person with mpox spots, their body fluids, respiratory droplets and contaminated objects such as bedding.[3] This includes close contact during sex.[21] Person-to-person spread of mpox has been recognised as a significant public health threat since the 2018 Nigerian outbreak.[19] Spread in hospital settings and household settings are well documented.[19] Risk factors for transmission include sharing a bed or room, or using the same utensils as an infected person.[45] Other risk factors noted in Africa include living in forested or recently deforested areas, no smallpox vaccination, handling or eating dead bush meat or monkeys, and sleeping on the floor.[40] Spread can occur by small droplets containing the virus, and whether it may spread through the air has not been ruled out.[15] People can transmit the virus from the onset of symptoms, and generally remain infectious until all the lesions have scabbed and fallen off.[2] However, an analysis of cases in the UK between 2018 and 2021, identified shedding of Monkeypox virus DNA in upper respiratory tract for a significant duration after crusting of all lesions, from three of the seven studied cases.[19] The duration of symptoms is typically 2 to 4 weeks.[5]
The virus enters the body through the nose, mouth, eyes or break in the skin, even if not visible.[47] It then replicates and spreads to local lymph nodes.[41]
People under the age of around 50 years may be particularly more at risk to mpox due to routine smallpox vaccination being discontinued following the eradication of smallpox.[27] Hunters in the tropical forests of Central and West Africa are most at risk.[7]
Diagnosis
Diagnosis can be verified by testing for the virus from a skin lesion.[3] This can be done by electron microscopy or PCR of the blister fluid, or viral culture.[26] A positive result does not always confirm mpox with certainty; it can also be positive if previous smallpox or vaccinia vaccine or with other orthopoxviruses.[3] The virus does not remain very long in the blood, and hence blood testing may not detect the disease.[3] Test results are interpreted together with symptoms.[3] The type can be identified by genomic sequencing.[26] Blood tests may show raised white blood cells and liver enzymes.[40]
Differential diagnosis
The rash of mpox looks identical to the rash of previously seen smallpox.[48] It may be mistaken for chickenpox.[12] Other illnesses that may appear similar include measles, scabies, bacterial skin infections, syphilis and reactions to some medicines.[3] Gonococcal septicaemia, lymphogranuloma venereum, chancroid and granuloma inguinale may also appear similar to mpox.[26]
Chickenpox
There are several key differences between mpox and chickenpox.[49] Early symptoms of chickenpox are typically mild.[4] The fever is not as high as in mpox.[49] Swollen lymph glands are prominent in mpox.[49] Lesions on the palms of the hands and soles of the feet are a feature in mpox and not characteristic of chickenpox.[49] Mpox lesions are firm, deep, more discrete and have a central dent.[49] It usually appears at varying stages of development in the same parts of the body and evolve slowly with each stage, lasting a day or 2.[42][49] Chickenpox lesions are usually more superficial in appearance with irregular borders, can be present at several stages on any one part on the body, and take a day or two to evolve from flat marks to the crust stage.[49] The distribution of chickenpox lesions usually starts on the trunk before spreading outwards, whereas in mpox, it more typically begins in the mouth and face before reaching out to hands and feet.[4] Both chickenpox and mpox may occur together in the same person.[49]
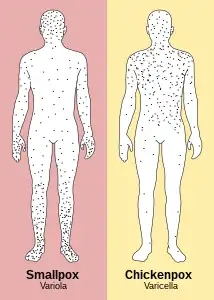 Smallpox (similar distribution to mpox) versus chickenpox
Smallpox (similar distribution to mpox) versus chickenpox Left: mpox Right: Orf
Left: mpox Right: Orf
Prevention

Previously, the smallpox vaccine has been shown to give around 85% protection in preventing infection in contacts and it lessened the severity of the disease.[4] Preventive measures include washing hands regularly and keeping away from sick people and other animals.[25] Where available, the MVA-BN smallpox vaccine, also known as Jynneos, Imvamune and Imvanex, may be offered to close contacts or those at high risk.[9] Two doses given by injection just under the skin are required for full vaccination.[9] It may be offered within 4 days of exposure, although it can be considered up to 14 days.[19] Unlike the traditional smallpox vaccine, MVA-BN does not leave a mark behind.[9] Where available, ACAM2000, given via a bifurcated needle is an alternative smallpox vaccine.[9]
Activities that may free up dried material from the skin spots, such as fans, dry dusting, brushing the floor, or vacuuming should be avoided.[10] If known to be in contact with an affected person, staying away from other people and watching for symptoms, may help reduce spread.[36] Although unclear whether the virus can spread via genital excretions, the use of condoms for 2-months after infection is recommended in addition to avoiding sex while symptomatic.[50]
Treatment
Tecovirimat, initially developed for smallpox, was approved for use in mpox in 2022, but is not widely avaialble.[3] Cidofovir or brincidofovir may be useful.[24] Other measures include the smallpox vaccine (MVA-BN), and vaccinia immune globulin (VIG).[11][14] The smallpox vaccine can also be used after being exposed to the mpox virus.[12]
Outcome

After healing, they may leave pale marks before becoming darker scars.[4] The risk of death in those infected ranges from 0% to 11%, depending on the type of mpox.[3][27] Fatality rates have been reported as around 3.6% in West Africa and 10.6% in Central Africa.[27] Most reported deaths have occurred in young children and people with HIV.[19]
Epidemiology
The disease has a changing epidemiology and is no longer as rare as previously thought;[13] possibly as a result of waning herd immunity since the cessation of routine smallpox vaccination.[23] Outbreaks have increasingly been occurring in more densely populated centres.[19] The highest rates of the disease in Africa have historically been in children who had not received smallpox vaccination.[31] More people being nearer to infected animals due to changes in land use, may also be a factor in the increasing rates in Africa.[31] Published mortality rates vary considerably and reflect sampling bias.[19]
The true number of people affected is not known due to the limited availability of testing worldwide.[4] Between 2003 and 2019, the disease was reported in four countries outside Africa, and the average age of presentation has increased from around age 4-years in the 1970s to 21-years in 2019.[51] Small viral outbreaks with secondary human-to-human infection occur routinely in Central and West Africa.[46] Cases have significantly increased since the 1980s.[28] In the US, evidence has been found of exposure to mpox in people without symptoms.[16]
It is highly endemic in the Democratic Republic of Congo,[27] where along with Nigeria, most cases occur.[12] Nigeria has been experiencing a large outbreak since 2017, with more than 500 suspected cases and over 200 confirmed cases.[3][52] Prior to 2017, it had not seen cases since 1978.[53][54] As of 2022, mpox is also endemic in Benin, Cameroon, the Central African Republic, Gabon, Ghana, Côte d’Ivoire, Liberia and Sierra Leone.[39] Since mid-May 2022, cases of mpox have been reported with person-to-person spread in close contacts, in several countries that do not have endemic mpox virus in animal or human populations, including countries in Europe, North America and Australasia.[50]
Between September 2009 and April 2014, around 12% of suspected mpox cases in Central Africa were confirmed as also having co-infection with chickenpox.[49] On 23, July 2022, the World Health Organization declared the 2022 mpox outbreak a Public Health Emergency of International Concern.[33] This has been done by the WHO few times, including the COVID-19 pandemic and Western African Ebola virus epidemic.[33]
History
Between 1958 and 1968, mainly for the purpose of producing and testing the polio vaccine, a small number of primates were being imported from Africa to Europe and the US, but most were from Asia.[55] During transit, there were often other wild animals and spread of infection had many opportunities.[55] In 1958, Preben von Magnus first identified mpox as a distinct pox illness in two non-fatal outbreaks in laboratory cynomolgus monkeys at the State Serum Institute, Copenhagen, Denmark, 51 and 62 days after the shipments arrived from Singapore by air.[29][56] Subsequent investigations detected the mpox virus in the kidneys of some monkeys that had no symptoms and were otherwise healthy.[57] The virus was never found in Asia, and the occurrence in Asian monkeys was likely due to contracting the disease in captivity and transit, or contamination.[55] Some previous pox illnesses among monkeys, assumed to be smallpox, may have been mpox.[29] During the 1960s, mpox was detected in several laboratory monkeys in Europe and the US, including in 1962 at the Walter Reed Army Institute of Research, where following exposure, several monkeys had antibodies but no symptoms.[57] No further cases in laboratory monkeys occurred after 1968 as conditions for monkeys improved and the requirement for monkeys from Asia and Africa, fell.[55] Until the outbreak of monkeypox at Rotterdam Zoo in 1964, mpox was thought to occur only in primates.[58] There, Central/South American giant anteaters first developed the disease before several orangutans, chimpanzees, gorillas, guenons, squirrel monkeys, macaques, marmosets and gibbons, and 11 of the 23 animals died.[57] The disease was particularly severe in orangutans.[59] At the time, mpox virus was also isolated from kidneys of healthy monkeys, but later found to be most likely due to contamination by the Zoo samples that were being looked at at the same laboratory.[55][57]
The first documented cases in humans was in 1970, in six unvaccinated children during the smallpox eradication efforts; the first being a 9-month old boy in the Democratic Republic of the Congo (formerly Zaire).[27][57] The others, including three who were playmates, were in Liberia and Sierra Leone.[57] It was noted to be less easily transmissible than smallpox.[4] From 1981 to 1986, over 300 cases of human mpox were reported in the DRC, the majority being due to contact with animals.[46] In 1996, the disease reemerged in the DRC with 88% of cases resulting from human-to-human transmission.[4] In humans, the disease remained confined to the rain forests of Western and Central Africa until 2003, when an outbreak of mpox occurred in the US.[60] All cases were traced to sick rodents, including Gambian pouched rats, imported from Ghana.[4] Local prairie dogs caught the infection and passed it onto their owners.[4] The disease was found to be mild and there were no deaths.[4] Between 1970 and 2019 the disease was reported in 10 African countries; mostly in Central and West Africa.[27]
In 2018, cases of mpox were diagnosed in the UK in two unrelated travellers from Nigeria.[61] That year the first human-to-human transmission outside of Africa was confirmed in the UK.[32] This person was a healthcare worker who possibly contracted the disease from contaminated bedlinen.[61] Cases were also reported in travellers to Israel and Singapore.[32] The UK saw further cases in 2019 and 2021.[12]
 Mpox in Liberia (1971)
Mpox in Liberia (1971) Mpox outbreak in DRC (1997)
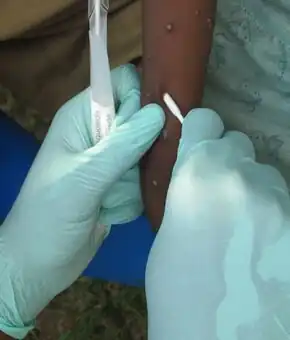
Mpox outbreak in DRC (1997) Testing of Gambian rats (1997)
Testing of Gambian rats (1997) Educational meeting DRC (1997)
Educational meeting DRC (1997)_-_CDC.png.webp) Mpox virion (2003 prairie dog outbreak)
Mpox virion (2003 prairie dog outbreak)
Society and culture
The Congo Basin clade, like smallpox, is designated a select agent.[4] In 2013 the West African type was declassified a select agent.[4] The disease burden is particularly high in Africa,[40] where it affects some of the world's poorest and most socially excluded communities.[19]
In the US there are regulations to control the importation of rodents from Africa.[62] The MVA-BN vaccine has generally been available in some countries who have placed large orders.[51] It was licensed in the UK in 2019.[26]
Abusive language during the 2022 outbreak has led the WHO to recommend replacing the term monkeypox with mpox.[35]
Other animals


Signs and symptoms in animals vary among different species.[63] The disease has been reported in dormice, prairie dogs, rabbits, squirrels and non-human primates, among other animals.[3][64]
Mpox infected Gambian pouched rats may have mild symptoms.[64] During the 2003 US outbreak, affected prairie dogs presented with fever, cough, sore eyes, poor feeding and rash.[63] Non-human primates present similarly.[63] They may have breathing problems, facial swelling, mouth ulcers and swollen glands.[64] In cynomolgus monkeys, the time from exposure to symptoms was noted to be around a week.[64] Rabbits and rodents typically present with fever, cough, runny nose, sore eyes and swollen glands.[64] They develop small bumps that fill with yellow fluid and may have patches of hair loss and pneumonia.[64] The disease has also been reported in dormice, tree squirrels and rope squirrels.[3] Other animals are likely susceptible but not known.[64]
Spread among other animals occurs via the fecal-oral route and through the nose, through wounds and eating infected meat.[64] Death is more likely in baby monkeys.[64] The CDC recommend that animals exposed to mpox are quarantined for six weeks.[64]
References
- 1 2 "Monkeypox in the U.S." Centers for Disease Control and Prevention. CDC. 22 July 2022. Archived from the original on 15 October 2017. Retrieved 29 July 2022.
- 1 2 3 4 5 6 "Clinical Recognition". www.cdc.gov. 23 May 2022. Archived from the original on 30 May 2022. Retrieved 31 May 2022.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 "Monkeypox". www.who.int. World Health Organization. 19 May 2022. Archived from the original on 21 April 2022. Retrieved 22 May 2022.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 Petersen, Brett W.; Damon, Inger K. (2020). "348. Smallpox, monkeypox and other poxvirus infections". In Goldman, Lee; Schafer, Andrew I. (eds.). Goldman-Cecil Medicine. Vol. 2 (26th ed.). Philadelphia: Elsevier. pp. 2180–2183. ISBN 978-0-323-53266-2. Archived from the original on 2022-05-23. Retrieved 2022-05-23.
- 1 2 3 4 "Monkeypox: signs and symptoms". CDC. 16 July 2021. Archived from the original on 23 May 2022. Retrieved 23 May 2022.
- 1 2 3 Petersen, Eskild; Kantele, Anu; Koopmans, Marion; Asogun, Danny; Yinka-Ogunleye, Adesola; Ihekweazu, Chikwe; Zumla, Alimuddin (December 2019). "Human Monkeypox: Epidemiologic and Clinical Characteristics, Diagnosis, and Prevention". Infectious Disease Clinics of North America. 33 (4): 1027–1043. doi:10.1016/j.idc.2019.03.001. ISSN 1557-9824. PMID 30981594. Archived from the original on 2021-11-06. Retrieved 2022-05-11.
- 1 2 3 "Part II: Monkeypox". Managing epidemics: Key facts about major deadly diseases. World Health Organization. 2018. pp. 172–179. ISBN 978-92-4-156553-0. Archived from the original on 2022-05-24. Retrieved 2022-05-24.
- 1 2 3 "2003 U.S. Outbreak Monkeypox". CDC. 11 May 2015. Archived from the original on 15 October 2017. Retrieved 15 October 2017.
- 1 2 3 4 5 6 "Monkeypox and Smallpox Vaccine Guidance | Monkeypox | Poxvirus". www.cdc.gov. 29 November 2019. Archived from the original on 19 May 2022. Retrieved 20 May 2022.
- 1 2 3 4 "Infection Control: Hospital | Monkeypox | Poxvirus | CDC". www.cdc.gov. 22 May 2022. Archived from the original on 18 May 2022. Retrieved 24 May 2022.
- 1 2 3 "Interim Clinical Guidance for the Treatment of Monkeypox | Monkeypox | Poxvirus | CDC". www.cdc.gov. 26 May 2022. Archived from the original on 7 June 2022. Retrieved 8 June 2022.
- 1 2 3 4 5 6 7 8 "Monkeypox". GOV.UK. 24 May 2022. Archived from the original on 18 May 2022. Retrieved 28 May 2022.
- 1 2 3 Simpson, Karl; Heymann, David; Brown, Colin S.; Edmunds, W. John; Elsgaard, Jesper; Fine, Paul; Hochrein, Hubertus; Hoff, Nicole A.; Green, Andrew; Ihekweazu, Chikwe; Jones, Terry C.; Lule, Swaib; Maclennan, Jane; McCollum, Andrea; Mühlemann, Barbara; Nightingale, Emily; Ogoina, Dimie; Ogunleye, Adesola; Petersen, Brett; Powell, Jacqueline; Quantick, Ollie; Rimoin, Anne W.; Ulaeato, David; Wapling, Andy (14 July 2020). "Human monkeypox - After 40 years, an unintended consequence of smallpox eradication". Vaccine. 38 (33): 5077–5081. doi:10.1016/j.vaccine.2020.04.062. ISSN 1873-2518. PMID 32417140. Archived from the original on 16 July 2021. Retrieved 10 May 2022.
- 1 2 3 4 5 "Monkeypox - United Kingdom of Great Britain and Northern Ireland". www.who.int. Archived from the original on 19 May 2022. Retrieved 19 May 2022.
- 1 2 3 4 5 6 "Multi-country monkeypox outbreak: situation update". www.who.int. World Health Organization. 4 June 2022. Archived from the original on 6 June 2022. Retrieved 7 June 2022.
- 1 2 3 Sutcliffe, Catherine G.; Rimone, Anne W.; Moss, William J. (2020). "32.2. Poxviruses". In Ryan, Edward T.; Hill, David R.; Solomon, Tom; Aronson, Naomi; Endy, Timothy P. (eds.). Hunter's Tropical Medicine and Emerging Infectious Diseases E-Book (Tenth ed.). Edinburgh: Elsevier. pp. 272–277. ISBN 978-0-323-55512-8. Archived from the original on 2022-06-10. Retrieved 2022-06-05.
- 1 2 Harris, Emily (27 May 2022). "What to Know About Monkeypox". JAMA. doi:10.1001/jama.2022.9499. ISSN 0098-7484. PMID 35622356. Archived from the original on 10 June 2022. Retrieved 6 June 2022.
- ↑ "Multi-country monkeypox outbreak: situation update". www.who.int. World Health Organization. Archived from the original on 14 June 2022. Retrieved 14 June 2022.
- 1 2 3 4 5 6 7 8 9 10 Adler, Hugh; Gould, Susan; Hine, Paul; Snell, Luke B.; Wong, Waison; Houlihan, Catherine F.; Osborne, Jane C.; Rampling, Tommy; Beadsworth, Mike Bj; Duncan, Christopher Ja; Dunning, Jake; Fletcher, Tom E.; Hunter, Ewan R.; Jacobs, Michael; Khoo, Saye H.; Newsholme, William; Porter, David; Porter, Robert J.; Ratcliffe, Libuše; Schmid, Matthias L.; Semple, Malcolm G.; Tunbridge, Anne J.; Wingfield, Tom; Price, Nicholas M. (24 May 2022). "Clinical features and management of human monkeypox: a retrospective observational study in the UK". The Lancet. Infectious Diseases: S1473–3099(22)00228–6. doi:10.1016/S1473-3099(22)00228-6. ISSN 1474-4457. PMID 35623380. Archived from the original on 29 May 2022. Retrieved 6 June 2022.
- 1 2 "Transmission Monkeypox". CDC. 11 May 2015. Archived from the original on 15 October 2017. Retrieved 15 October 2017.
- 1 2 "Monkeypox: public health advice for gay, bisexual and other men who have sex with men". www.who.int. 26 May 2022. Archived from the original on 26 May 2022. Retrieved 27 May 2022.
- ↑ "Smallpox & Other Orthopoxvirus-Associated Infections - Chapter 4 - 2020 Yellow Book | Travelers' Health | CDC". wwwnc.cdc.gov. Archived from the original on 29 July 2022. Retrieved 29 July 2022.
- 1 2 3 McCollum AM, Damon IK (January 2014). "Human monkeypox". Clinical Infectious Diseases. 58 (2): 260–7. doi:10.1093/cid/cit703. PMID 24158414.
- 1 2 "Treatment | Monkeypox | Poxvirus | CDC". www.cdc.gov. 28 December 2018. Archived from the original on 15 June 2019. Retrieved 11 October 2019.
- 1 2 "Prevention". www.cdc.gov. 29 November 2019. Archived from the original on 14 March 2022. Retrieved 14 May 2022.
- 1 2 3 4 5 6 7 Gilbourne, Marika; Coulson, Ian; Mitchell, Gus (May 2022). Amanda Oakley (ed.). "Monkeypox: Symptoms, Treatment, and Outcome — DermNet". dermnetnz.org. Archived from the original on 13 August 2021. Retrieved 25 May 2022.
- 1 2 3 4 5 6 7 8 Bunge, Eveline M.; Hoet, Bernard; Chen, Liddy; Lienert, Florian; Weidenthaler, Heinz; Baer, Lorraine R.; Steffen, Robert (11 February 2022). "The changing epidemiology of human monkeypox—A potential threat? A systematic review". PLOS Neglected Tropical Diseases. 16 (2): e0010141. doi:10.1371/journal.pntd.0010141. ISSN 1935-2735. Archived from the original on 22 February 2022. Retrieved 9 May 2022.
- 1 2 James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2020). "19. Viral diseases". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Edinburgh: Elsevier. p. 389. ISBN 978-0-323-54753-6. Archived from the original on 2022-05-11. Retrieved 2022-05-11.
- 1 2 3 Arita, I; Henderson, A (1968). "Smallpox and Monkeypox in Non-human Primates" (PDF). Bulletin of the World Health Organization. pp. 277–283. Archived (PDF) from the original on 24 May 2022. Retrieved 29 September 2018.
- ↑ "Monkeypox". CDC. 11 May 2015. Archived from the original on 15 October 2017. Retrieved 15 October 2017.
- 1 2 3 Adalja, Amesh; Inglesby, Tom (24 May 2022). "A Novel International Monkeypox Outbreak". Annals of Internal Medicine. doi:10.7326/M22-1581. ISSN 0003-4819. Archived from the original on 27 May 2022. Retrieved 1 June 2022.
- 1 2 3 Mauldin, Matthew R.; McCollum, Andrea M.; Nakazawa, Yoshinori J.; Mandra, Anna; Whitehouse, Erin R.; Davidson, Whitni; Zhao, Hui; Gao, Jinxin; Li, Yu; Doty, Jeffrey; Yinka-Ogunleye, Adesola; Akinpelu, Afolabi; Aruna, Olusola; Naidoo, Dhamari; Lewandowski, Kuiama; Afrough, Babak; Graham, Victoria; Aarons, Emma; Hewson, Roger; Vipond, Richard; Dunning, Jake; Chand, Meera; Brown, Colin; Cohen-Gihon, Inbar; Erez, Noam; Shifman, Ohad; Israeli, Ofir; Sharon, Melamed; Schwartz, Eli; Beth-Din, Adi; Zvi, Anat; Mak, Tze Minn; Ng, Yi Kai; Cui, Lin; Lin, Raymond T. P.; Olson, Victoria A.; Brooks, Tim; Paran, Nir; Ihekweazu, Chikwe; Reynolds, Mary G. (19 April 2022). "Exportation of Monkeypox Virus From the African Continent". The Journal of Infectious Diseases. 225 (8): 1367–1376. doi:10.1093/infdis/jiaa559. ISSN 1537-6613. PMID 2880628. Archived from the original on 19 May 2022. Retrieved 25 May 2022.
- 1 2 3 "WHO declares monkeypox a global public health emergency". NBC News. Archived from the original on 23 July 2022. Retrieved 23 July 2022.
- ↑ "Mpox is no longer a global health emergency, WHO declares - National | Globalnews.ca". Global News. Archived from the original on 11 May 2023. Retrieved 11 May 2023.
- 1 2 "WHO recommends new name for monkeypox disease". www.who.int. Archived from the original on 1 December 2022. Retrieved 2 December 2022.
- 1 2 "Multi-country monkeypox outbreak in non-endemic countries: Update". www.who.int. 29 May 2022. Archived from the original on 30 May 2022. Retrieved 30 May 2022.
- 1 2 Reed, KD; Melski, JW; Graham, MB; Regnery, RL; Sotir, MJ; Wegner, MV; Kazmierczak, JJ; Stratman, EJ; Li, Y; Fairley, JA; Swain, GR; Olson, VA; Sargent, EK; Kehl, SC; Frace, MA; Kline, R; Foldy, SL; Davis, JP; Damon, IK (22 January 2004). "The detection of monkeypox in humans in the Western Hemisphere". The New England journal of medicine. 350 (4): 342–50. doi:10.1056/NEJMoa032299. ISSN 1533-4406. PMID 14736926. Archived from the original on 5 June 2022. Retrieved 6 June 2022.
- ↑ Caldas, JP; Valdoleiros, SR; Rebelo, S; Tavares, M (17 October 2022). "Monkeypox after Occupational Needlestick Injury from Pustule". Emerging infectious diseases. 28 (12). doi:10.3201/eid2812.221374. PMID 36252152.
- 1 2 "Monkeypox". www.who.int. World Health Organization. Archived from the original on 24 May 2022. Retrieved 25 May 2022.
- 1 2 3 4 5 6 Brown, K; Leggat, PA (20 December 2016). "Human Monkeypox: Current State of Knowledge and Implications for the Future". Tropical medicine and infectious disease. 1 (1). doi:10.3390/tropicalmed1010008. PMID 30270859. Archived from the original on 20 May 2022. Retrieved 6 June 2022.
- 1 2 Moore, M; Zahra, F (22 May 2022). "Monkeypox". StatPearls. StatPearls Publishing. PMID 34662033. Archived from the original on 25 May 2022. Retrieved 27 May 2022.
- 1 2 Macneil, A; Reynolds, MG; Braden, Z; Carroll, DS; Bostik, V; Karem, K; Smith, SK; Davidson, W; Li, Y; Moundeli, A; Mombouli, JV; Jumaan, AO; Schmid, DS; Regnery, RL; Damon, IK (1 January 2009). "Transmission of atypical varicella-zoster virus infections involving palm and sole manifestations in an area with monkeypox endemicity". Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 48 (1): 1–16. doi:10.1086/595552. PMID 19025497. Archived from the original on 26 May 2022. Retrieved 3 June 2022.
- ↑ "Transmission". www.cdc.gov. 11 May 2015. Archived from the original on 24 May 2022. Retrieved 24 May 2022.
- 1 2 Falendysz EA, Lopera JG, Lorenzsonn F, Salzer JS, Hutson CL, Doty J, et al. (2015-10-30). "Further Assessment of Monkeypox Virus Infection in Gambian Pouched Rats (Cricetomys gambianus) Using In Vivo Bioluminescent Imaging". PLOS Neglected Tropical Diseases. 9 (10): e0004130. doi:10.1371/journal.pntd.0004130. PMC 4627722. PMID 26517839.
- 1 2 Kantele A, Chickering K, Vapalahti O, Rimoin AW (August 2016). "Emerging diseases-the monkeypox epidemic in the Democratic Republic of the Congo". Clinical Microbiology and Infection. 22 (8): 658–9. doi:10.1016/j.cmi.2016.07.004. PMID 27404372.
- 1 2 3 Meyer H, Perrichot M, Stemmler M, Emmerich P, Schmitz H, Varaine F, et al. (August 2002). "Outbreaks of disease suspected of being due to human monkeypox virus infection in the Democratic Republic of Congo in 2001". Journal of Clinical Microbiology. 40 (8): 2919–21. doi:10.1128/JCM.40.8.2919-2921.2002. PMC 120683. PMID 12149352.
- ↑ "Monkeypox fact sheet for primary care" (PDF). GOV.UK. December 2019. Archived (PDF) from the original on 16 May 2022. Retrieved 29 May 2022.
- ↑ Barlow, Gavin; Irving, William L.; Moss, Peter J. (2020). "20. Infectious disease". In Feather, Adam; Randall, David; Waterhouse, Mona (eds.). Kumar and Clark's Clinical Medicine (10th ed.). Elsevier. p. 517. ISBN 978-0-7020-7870-5. Archived from the original on 2022-05-05. Retrieved 2022-05-09.
- 1 2 3 4 5 6 7 8 9 Hughes, Christine M.; Liu, Lindy; Davidson, Whitni B.; Radford, Kay W.; Wilkins, Kimberly; Monroe, Benjamin; Metcalfe, Maureen G.; Likafi, Toutou; Lushima, Robert Shongo; Kabamba, Joelle; Nguete, Beatrice; Malekani, Jean; Pukuta, Elisabeth; Karhemere, Stomy; Muyembe Tamfum, Jean-Jacques; Okitolonda Wemakoy, Emile; Reynolds, Mary G.; Schmid, D. Scott; McCollum, Andrea M. (3 February 2021). "A Tale of Two Viruses: Coinfections of Monkeypox and Varicella Zoster Virus in the Democratic Republic of Congo". The American Journal of Tropical Medicine and Hygiene. 104 (2): 604–611. doi:10.4269/ajtmh.20-0589.
- 1 2 "Principles for monkeypox control in the UK: 4 nations consensus statement". GOV.UK. Archived from the original on 30 May 2022. Retrieved 31 May 2022.
- 1 2 "Meeting proceedings". WHO Advisory Committee on Variola Virus Research: report of the twenty-third meeting, virtual meeting, 3-4 November 2021. World Health Organization. 2022. pp. 14–18. ISBN 978-92-4-004674-0. Archived from the original on 20 May 2022. Retrieved 20 May 2022.
- ↑ Phoobane, Paulina; Masinde, Muthoni; Mabhaudhi, Tafadzwanashe (8 February 2022). "Predicting Infectious Diseases: A Bibliometric Review on Africa". International Journal of Environmental Research and Public Health. 19 (3): 1893. doi:10.3390/ijerph19031893. ISSN 1660-4601. PMID 35162917. Archived from the original on 25 May 2022. Retrieved 25 May 2022.
- ↑ Yinka-Ogunleye, Adesola; Aruna, Olusola; Dalhat, Mahmood; Ogoina, Dimie; McCollum, Andrea; Disu, Yahyah; Mamadu, Ibrahim; Akinpelu, Afolabi; Ahmad, Adama; Burga, Joel; Ndoreraho, Adolphe; Nkunzimana, Edouard; Manneh, Lamin; Mohammed, Amina; Adeoye, Olawunmi; Tom-Aba, Daniel; Silenou, Bernard; Ipadeola, Oladipupo; Saleh, Muhammad; Adeyemo, Ayodele; Nwadiutor, Ifeoma; Aworabhi, Neni; Uke, Patience; John, Doris; Wakama, Paul; Reynolds, Mary; Mauldin, Matthew R.; Doty, Jeffrey; Wilkins, Kimberly; Musa, Joy; Khalakdina, Asheena; Adedeji, Adebayo; Mba, Nwando; Ojo, Olubunmi; Krause, Gerard; Ihekweazu, Chikwe (August 2019). "Outbreak of human monkeypox in Nigeria in 2017-18: a clinical and epidemiological report". The Lancet. Infectious Diseases. 19 (8): 872–879. doi:10.1016/S1473-3099(19)30294-4. ISSN 1474-4457. PMID 31285143. Archived from the original on 2022-06-03. Retrieved 2022-06-05.
- ↑ Breman JG, Kalisa R, Steniowski MV, Zanotto E, Gromyko AI, Arita I (1980). "Human monkeypox, 1970-79". Bull World Health Organ. 58 (2): 165–182. PMC 2395797. PMID 6249508.
- 1 2 3 4 5 Fenner, Frank; Wittek, Riccardo; Dumbell, Keith R. (1988). "8. Monkeypox virus". The Orthopoxviruses. Elsevier. pp. 227–267. ISBN 978-0-323-15022-4. Archived from the original on 2022-05-26. Retrieved 2022-05-26.
- ↑ Fenner, Frank; Wittek, Riccardo; Dumbell, Keith R. (1988). "1. Historical introduction and overview". The Orthopoxviruses. Elsevier. pp. 11–12. ISBN 978-0-323-15022-4. Archived from the original on 2022-05-26. Retrieved 2022-05-26.
- 1 2 3 4 5 6 Cho, C. T.; Wenner, H. A. (March 1973). "Monkeypox virus". Bacteriological Reviews. 37 (1): 1–18. doi:10.1128/br.37.1.1-18.1973. ISSN 0005-3678. PMID 4349404. Archived from the original on 2022-05-12. Retrieved 2022-05-27.
- ↑ Reynolds, Mary G.; Damon, Inger K. (2017). Cockerham, William C. (ed.). International Encyclopedia of Public Health. Vol. 6 (2nd ed.). Oxford: Elsevier. pp. 529–530. ISBN 978-0-12-803678-5. Archived from the original on 2022-06-10. Retrieved 2022-05-30.
- ↑ Essbauer, Sandra; Meyer, Herman (2007). "Genus Orthopoxvirus: Monkeypox virus". In Mercer, Andrew; Schmidt, Axel; Weber, Olaf (eds.). Poxviruses. Springer. p. 66. ISBN 3-7643-7556-6. Archived from the original on 2022-05-30. Retrieved 2022-05-30.
- ↑ Graham, Mary beth (26 September 2019). "Monkeypox: Background, Pathophysiology, Etiology". emedicine.medscape.com. Archived from the original on 6 January 2022. Retrieved 10 May 2022.
- 1 2 Vaughan, A; Aarons, E; Astbury, J; Brooks, T; Chand, M; Flegg, P; Hardman, A; Harper, N; Jarvis, R; Mawdsley, S; McGivern, M; Morgan, D; Morris, G; Nixon, G; O'Connor, C; Palmer, R; Phin, N; Price, DA; Russell, K; Said, B; Schmid, ML; Vivancos, R; Walsh, A; Welfare, W; Wilburn, J; Dunning, J (April 2020). "Human-to-Human Transmission of Monkeypox Virus, United Kingdom, October 2018". Emerging infectious diseases. 26 (4): 782–785. doi:10.3201/eid2604.191164. PMID 32023204. Archived from the original on 2022-05-24. Retrieved 2022-05-30.
- ↑ "African Rodent Importation Ban". www.cdc.gov. 11 May 2015. Archived from the original on 18 May 2022. Retrieved 24 May 2022.
- 1 2 3 "Examining Animals With Suspected Monkeypox | Monkeypox | Poxvirus | CDC". www.cdc.gov. CDC. 19 November 2019. Archived from the original on 19 May 2022. Retrieved 24 May 2022.
- 1 2 3 4 5 6 7 8 9 10 Nash, Sherrie L.; Palmer, Sally B.; Wingfield, Wayne E. (2009). "1.11. Zoonoses and zoonotic diseases". In Wingfield, Wayne E.; Palmer, Sally B. (eds.). Veterinary Disaster Response. Iowa: John Wiley & Sons. pp. 167–168. ISBN 978-0-8138-1014-0.
External links
- "Mpox". www.who.int. World Health Organization. Archived from the original on 24 May 2022. Retrieved 25 May 2022.
- "Mpox". www.cdc.gov. CDC. 7 June 2022. Archived from the original on 15 October 2017. Retrieved 8 June 2022.
- "Monkeypox". GOV.UK. UK Health Security Agency. Archived from the original on 18 May 2022. Retrieved 8 June 2022.
- "Mpox vaccine". Guy's and St Thomas' NHS Foundation Trust. Archived from the original on 4 December 2022. Retrieved 4 December 2022.
| Classification |
|---|