Niraparib
 | |
| Names | |
|---|---|
| Pronunciation | /nɪˈræpərɪb/ nih-RAP-uh-rib |
| Trade names | Zejula |
| Other names | Niraparib tosylate, MK-4827 |
IUPAC name
| |
| Clinical data | |
| Drug class | Poly ADP-ribose polymerase (PARP) inhibitor[1] |
| Main uses | Epithelial ovarian, fallopian tube, or primary peritoneal cancer[1] |
| Side effects | Nausea, low platelets, tiredness, low red blood cells, constipation, abdominal pain, low white blood cells, trouble sleeping, headache, diarrhea, shortness of breath, high blood pressure, joint pain, hot flushes[2] |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Pregnancy category |
|
| Routes of use | By mouth |
| Typical dose | 200 to 300 mg OD[1] |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a617007 |
| Legal | |
| License data | |
| Legal status | |
| Pharmacokinetics | |
| Bioavailability | 73% |
| Protein binding | 83% |
| Metabolism | Carboxylesterases |
| Metabolites | M1 (carboxylic acid) |
| Elimination half-life | 36 hours |
| Excretion | 48% urine, 29% feces |
| Chemical and physical data | |
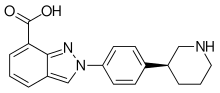
| Formula | C19H20N4O |
| Molar mass | 320.396 g·mol−1 |
| 3D model (JSmol) | |
| Solubility in water | 0.7–1.1 |
SMILES
| |
InChI
| |
Niraparib, sold under the brand name Zejula, is a medication used to treat epithelial ovarian, fallopian tube, or primary peritoneal cancer.[1][2] It is typically used after platinum-based chemotherapy.[4] It is taken by by mouth.[2]
Common side effects include nausea, low platelets, tiredness, low red blood cells, constipation, abdominal pain, low white blood cells, trouble sleeping, headache, diarrhea, shortness of breath, high blood pressure, joint pain, and hot flushes.[2] Other side effects may include myelodysplastic syndrome and infertility.[4] Use in pregnancy may harm the baby.[1] It is a poly ADP-ribose polymerase (PARP) inhibitor.[1]
Niraparib was approved for medical use in the United States and Europe in 2017.[2][4] In the United Kingdom 4 weeks of treatment at 200 mg per day costs the NHS about £4,500.[5] This amount in the United States costs about 16,300 USD.[6]
Medical uses
Niraparib is indicated for the maintenance treatment of adults with recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer who are in complete or partial response to platinum-based chemotherapy.[7]
In October 2019, the indication for niraparib was expanded to include people with advanced ovarian, fallopian tube, or primary peritoneal cancer treated with three or more prior chemotherapy regimens and whose cancer is associated with homologous recombination deficiency (HRD)-positive status.[8] HRD is defined by either a deleterious or suspected deleterious BRCA mutation, or genomic instability in patients with disease progression greater than six months after response to the last platinum-based chemotherapy.[8]
In April 2020, the indication for niraparib was expanded to include the maintenance treatment of adults with advanced epithelial ovarian, fallopian tube, or primary peritoneal cancer who are in a complete or partial response to first-line platinum-based chemotherapy.[9]
In the European Union, niraparib is indicated: as monotherapy for the maintenance treatment of adults with advanced epithelial (FIGO Stages III and IV) high-grade ovarian, fallopian tube or primary peritoneal cancer who are in response (complete or partial) following completion of first-line platinum-based chemotherapy; and as monotherapy for the maintenance treatment of adults with platinum sensitive relapsed high grade serous epithelial ovarian, fallopian tube, or primary peritoneal cancer who are in response (complete or partial) to platinum based chemotherapy.[2]
Dosage
It is generally taken at a dose of 200 to 300 mg once per day.[1] The lower dose is used in people under 58 kg.[5]
Contraindications
No contraindications are listed in the prescribing information.[1]
Side effects
The most common side effects in studies were low blood cell counts, namely thrombocytopenia (in 61% of patients, severe in 29%), anemia (in 50%, severe in 25%) and neutropenia (in 30%, severe in 20%). Other, mostly mild to moderate side effects included nausea, fatigue, and constipation. In a study running over 250 days (median), 15% of patients had to permanently discontinue niraparib due to adverse effects.[1]
Interactions
No clinical interaction studies have been performed. The potential for interactions with other drugs is low as niraparib and its main metabolite M1 do not significantly interact with any of the important cytochrome P450 liver enzymes in vitro. Niraparib, but not M1, is transported by P-glycoprotein and BCRP, but does not significantly inhibit them. Neither niraparib nor M1 significantly interact with any of the other important transporter proteins.[1]
Pharmacology
Mechanism of action
Niraparib is an inhibitor of the enzymes PARP1 and PARP2.[10]
Pharmacokinetics
73% of ingested niraparib is absorbed in the gut,[12] and it reaches highest blood plasma concentrations after about three hours, independently of food intake. In the circulation, 83% of the substance are bound to plasma proteins. It is inactivated by carboxylesterases to the main metabolite M1, the carboxylic acid derivative,[11] which is subsequently glucuronidated.[1]
The mean biological half-life is 36 hours. 47.5% of the substance are found in the urine and 38.8% in the feces. Unmetabolised niraparib accounts for 11% in the urine and 19% in the feces.[11]
Chemistry
The drug is used in form of the salt niraparib tosylate monohydrate, which is white to off-white, non-hygroscopic crystals.[1][10]
History
Niraparib was granted fast track designation by the US Food and Drug Administration (FDA), and Tesaro submitted a new drug application in 2016.[13] It was approved on 27 March 2017 in the US,[7] and approved in European Union on 16 November 2017.[14]
In a study with 553 patients, progression-free survival (PFS) for patients with a deleterious or suspected deleterious BRCA mutation in the germline was 21.0 months under niraparib therapy, as compared to 5.5 months under placebo. Patients without such a mutation had a PFS of 9.3 months under niraparib versus 3.9 months under placebo.[7][15]
The US Food and Drug Administration (FDA) granted the application for niraparib fast track, priority review, breakthrough therapy, and orphan drug designations.[7]
Research
A 2012 study in a cell line found that PARP inhibitors exhibit cytotoxic effects not based solely on their enzymatic inhibition of PARP, but by their trapping of PARP on damaged DNA, and the strength of this trapping activity was ordered niraparib >> olaparib >> veliparib.[16]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 "Zejula- niraparib capsule". DailyMed. Archived from the original on 24 March 2021. Retrieved 17 January 2021.
- 1 2 3 4 5 6 7 "Zejula EPAR". European Medicines Agency (EMA). Archived from the original on 13 November 2020. Retrieved 17 January 2021. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ↑ "Zejula 100 mg hard capsules - Summary of Product Characteristics (SmPC)". (emc). Archived from the original on 19 January 2021. Retrieved 17 January 2021.
- 1 2 3 "Niraparib Monograph for Professionals". Drugs.com. Archived from the original on 18 January 2021. Retrieved 13 November 2021.
- 1 2 BNF 81: March-September 2021. BMJ Group and the Pharmaceutical Press. 2021. p. 1050. ISBN 978-0857114105.
- ↑ "Zejula Prices, Coupons & Patient Assistance Programs". Drugs.com. Archived from the original on 26 January 2021. Retrieved 13 November 2021.
- 1 2 3 4 "Niraparib (Zejula)". U.S. Food and Drug Administration (FDA). 30 March 2017. Archived from the original on 15 August 2021. Retrieved 31 August 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - 1 2 "FDA approves niraparib for HRD-positive advanced ovarian cancer". U.S. Food and Drug Administration (FDA). 23 October 2019. Archived from the original on 22 December 2020. Retrieved 17 January 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ "FDA approves niraparib for first-line maintenance of advanced ovarian". U.S. Food and Drug Administration (FDA). 29 April 2020. Archived from the original on 17 January 2021. Retrieved 17 January 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - 1 2 "Niraparib Monograph for Professionals". American Society of Health-System Pharmacists. 22 September 2020. Archived from the original on 18 January 2021. Retrieved 17 January 2021.
- 1 2 3 van Andel L, Zhang Z, Lu S, Kansra V, Agarwal S, Hughes L, et al. (December 2017). "14C-niraparib, a novel poly(ADP-Ribose) polymerase (PARP)-1 and PARP-2 inhibitor, in patients with advanced cancer". Investigational New Drugs. 35 (6): 751–765. doi:10.1007/s10637-017-0451-2. PMC 5694528. PMID 28303528.
- ↑ van Andel L, Rosing H, Zhang Z, Hughes L, Kansra V, Sanghvi M, et al. (January 2018). "14C-microtracer and therapeutic dose in cancer patients". Cancer Chemotherapy and Pharmacology. 81 (1): 39–46. doi:10.1007/s00280-017-3455-x. PMC 5754411. PMID 29043410.
- ↑ "Niraparib Receives FDA Fast Track Designation for the Treatment of Recurrent Platinum-Sensitive Ovarian, Fallopian Tube, or Primary Peritoneal Cancer". The European Society for Medical Oncology (ESMO). 5 September 2016. Archived from the original on 4 August 2020. Retrieved 31 August 2021.
- ↑ "Zejula". European Medicines Agency. 17 September 2018. Archived from the original on 9 August 2018. Retrieved 14 March 2022.
- ↑ Adams B (29 June 2016). "Tesaro's PARP ovarian cancer drug hits PhIII goal; prepares to file". Fierce Biotech. Archived from the original on 15 August 2021. Retrieved 31 August 2021.
- ↑ Murai J, Huang SY, Das BB, Renaud A, Zhang Y, Doroshow JH, et al. (November 2012). "Trapping of PARP1 and PARP2 by Clinical PARP Inhibitors". Cancer Research. 72 (21): 5588–99. doi:10.1158/0008-5472.CAN-12-2753. PMC 3528345. PMID 23118055.
External links
| External sites: |
|
|---|---|
| Identifiers: |
- "Niraparib tosylate". Drug Information Portal. U.S. National Library of Medicine. Archived from the original on 15 August 2021. Retrieved 31 August 2021.
- "Niraparib tosylate monohydrate". NCI Drug Dictionary. National Cancer Institute. Archived from the original on 15 August 2021. Retrieved 31 August 2021.
- "Niraparib tosylate monohydrate". National Cancer Institute. 14 April 2017. Archived from the original on 15 August 2021. Retrieved 31 August 2021.