Omacetaxine
 | |
 | |
| Names | |
|---|---|
| Trade names | Synribo, Tekinex, others |
| Other names | Omacetaxine mepesuccinate, homoharringtonine (HHT) |
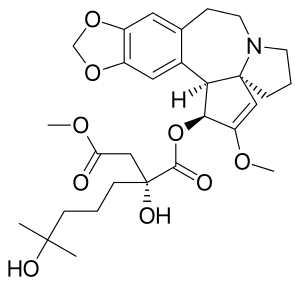
IUPAC name
| |
| Clinical data | |
| Drug class | Protein synthesis inhibitor[1] |
| Main uses | Chronic myeloid leukemia (CML)[1] |
| Side effects | Low platelets, low red blood cells, low white blood cells, fever, diarrhea, nausea, pain[1] |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Pregnancy category |
|
| Routes of use | Subcutaneous, intravenous infusion |
| Typical dose | 1.25 mg/m2[1] |
| External links | |
| AHFS/Drugs.com | Monograph |
| Legal | |
| License data | |
| Legal status |
|
| Pharmacokinetics | |
| Protein binding | 50% |
| Metabolism | Mostly via plasma esterases |
| Elimination half-life | 6 hours |
| Excretion | Urine (≤15% unchanged) |
| Chemical and physical data | |
| Formula | C29H39NO9 |
| Molar mass | 545.629 g·mol−1 |
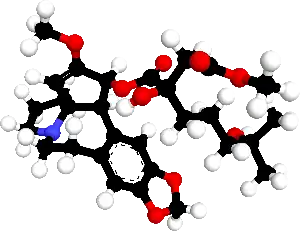
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Omacetaxine, sold under the brand name Synribo, is a medication used to treat chronic myeloid leukemia (CML).[1] It is used in cases were other medications have not worked.[1] It is given by injection under the skin.[1]
Common side effects include low platelets, low red blood cells, low white blood cells, fever, diarrhea, nausea, and pain.[1] Other side effects may include bleeding and infection.[1] Use during pregnancy may harm the baby.[1] It is a protein synthesis inhibitor.[1]
Omacetaxine was approved for medical use in the United States in 2012.[1] It is not approved in Europe.[2] In the United States it costs about 1,200 USD for 3.5 mg as of 2021.[3] It is made from a substance in the Chinese evergreen known as harringtonine.[2]
Medical uses
Omacetaxine is indicated for use as a treatment for people with chronic myeloid leukaemia who are resistant or intolerant of tyrosine kinase inhibitors.[4][5][6]
Dosage
The dose is 1.25 mg/m2.[1]
It is initially given twice per day for 2 weeks followed by 2 weeks off.[1]
In following rounds it is given for 1 week followed by 3 weeks off.[1]
Side effects
By frequency:[7][4]
Very common (>10% frequency):
- Diarrhoea
- Myelosuppression†
- Injection site reactions
- Nausea
- Fatigue
- Fever
- Muscle weakness
- Joint pain
- Headache
- Cough
- Hair loss
- Constipation
- Nosebleeds
- Upper abdominal pain
- Pain in the extremities
- Oedema
- Vomiting
- Back pain
- Hyperglycemia, sometimes extreme
- Gout
- Rash
- Insomnia
Common (1–10% frequency):
- Seizures
- Haemorrhage
† Myelosuppression, including: thrombocytopenia, anaemia, neutropenia and lymphopenia, in descending order of frequency.
Omacetaxine mepesuccinate can cause fetal harm when administered to a pregnant woman. Women using HHT should avoid becoming pregnant and also avoid nursing while receiving HHT.[8]
Mechanism of action
Omacetaxine is a protein translation inhibitor. It inhibits protein translation by preventing the initial elongation step of protein synthesis. It interacts with the ribosomal A-site and prevents the correct positioning of amino acid side chains of incoming aminoacyl-tRNAs. Omacetaxine acts only on the initial step of protein translation and does not inhibit protein synthesis from mRNAs that have already commenced translation.[9]
History
HHT is a natural plant alkaloid derived from Cephalotaxus fortunei. HHT and related compound esters of cephalotaxine were described first in 1970, and were the subject of intensive research efforts by Chinese investigators to clarify their role as anticancer and antileukemic agents from the 1970s until the present.[10]
Research
In June 2009, results of a long-term open label Phase II study were published, which investigated the use of omacetaxine infusions in CML patients. After twelve months of treatment, about one third of patients showed a cytogenetic response.[11] A study in patients who had failed imatinib and who had the drug resistant T315I mutation achieved cytogenetic response in 28% of patients and hematologic response in 80% of patients, according to preliminary data.[12]
Phase I studies including a small number of patients have shown benefit in treating myelodysplastic syndrome (MDS, 25 patients)[13] and acute myelogenous leukaemia (AML, 76 patients).[14] Patients with solid tumors did not benefit from omacetaxine.[15]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 "Omacetaxine Monograph for Professionals". Drugs.com. Archived from the original on 4 March 2021. Retrieved 7 November 2021.
- 1 2 "Tekinex". Archived from the original on 30 October 2020. Retrieved 7 November 2021.
- ↑ "Synribo Prices, Coupons & Patient Assistance Programs". Drugs.com. Retrieved 7 November 2021.
- 1 2 "SYNRIBO (omacetaxine mepesuccinate) injection, powder, lyophilized, for solution [Cephalon, Inc.]". DailyMed. Cephalon, Inc. October 2012. Archived from the original on 22 February 2014. Retrieved 18 February 2014.
- ↑ Sweetman, S, ed. (14 November 2012). "Omacetaxine Mepesuccinate". Martindale: The Complete Drug Reference. Medicines Complete. Pharmaceutical Press.
- ↑ Lacroix M (2014). Targeted Therapies in Cancer. Hauppauge , NY: Nova Sciences Publishers. ISBN 978-1-63321-687-7. Archived from the original on 2015-06-26. Retrieved 2014-07-13.
- ↑ "Synribo (omacetaxine) dosing, indications, interactions, adverse effects, and more". Medscape Reference. WebMD. Archived from the original on 21 February 2014. Retrieved 18 February 2014.
- ↑ "SYNRIBOTM (omacetaxine mepesuccinate) drug label" (PDF). FDA. Archived (PDF) from the original on 2021-04-08. Retrieved 2021-02-08.
- ↑ Wetzler M, Segal D (2011). "Omacetaxine as an anticancer therapeutic: what is old is new again". Current Pharmaceutical Design. 17 (1): 59–64. doi:10.2174/138161211795049778. PMID 21294709.
- ↑ Kantarjian HM, O'Brien S, Cortes J (October 2013). "Homoharringtonine/omacetaxine mepesuccinate: the long and winding road to food and drug administration approval". Clinical Lymphoma, Myeloma & Leukemia. 13 (5): 530–3. doi:10.1016/j.clml.2013.03.017. PMC 3775965. PMID 23790799.
- ↑ Li YF, Deng ZK, Xuan HB, Zhu JB, Ding BH, Liu XN, Chen BA (June 2009). "Prolonged chronic phase in chronic myelogenous leukemia after homoharringtonine therapy". Chinese Medical Journal. 122 (12): 1413–7. PMID 19567163.
- ↑ Quintás-Cardama A, Kantarjian H, Cortes J (December 2009). "Homoharringtonine, omacetaxine mepesuccinate, and chronic myeloid leukemia circa 2009". Cancer. 115 (23): 5382–93. doi:10.1002/cncr.24601. PMID 19739234.
- ↑ Wu L, Li X, Su J, Chang C, He Q, Zhang X, et al. (September 2009). "Effect of low-dose cytarabine, homoharringtonine and granulocyte colony-stimulating factor priming regimen on patients with advanced myelodysplastic syndrome or acute myeloid leukemia transformed from myelodysplastic syndrome". Leukemia & Lymphoma. 50 (9): 1461–7. doi:10.1080/10428190903096719. PMID 19672772. S2CID 10675425.
- ↑ Gu LF, Zhang WG, Wang FX, Cao XM, Chen YX, He AL, et al. (June 2011). "Low dose of homoharringtonine and cytarabine combined with granulocyte colony-stimulating factor priming on the outcome of relapsed or refractory acute myeloid leukemia". Journal of Cancer Research and Clinical Oncology. 137 (6): 997–1003. doi:10.1007/s00432-010-0947-z. PMID 21152934. S2CID 20406046.
- ↑ Kantarjian HM, Talpaz M, Santini V, Murgo A, Cheson B, O'Brien SM (September 2001). "Homoharringtonine: history, current research, and future direction". Cancer. 92 (6): 1591–605. doi:10.1002/1097-0142(20010915)92:6<1591::AID-CNCR1485>3.0.CO;2-U. PMID 11745238.
External links
| Identifiers: |
|
|---|