Carbidopa/levodopa
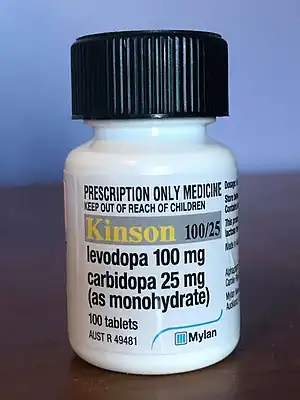 Bottle of carbidopa (25 mg) / levodopa (100 mg) in Australia. | |
| Combination of | |
|---|---|
| Agonist | Levodopa |
| Enzyme inhibitor | Carbidopa |
| Names | |
| Trade names | Atamet, Carbilev, Sinemet, others |
| Clinical data | |
| Main uses | Parkinson's disease[1] |
| Side effects | Movement problems, nausea[1] |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Pregnancy category |
|
| Defined daily dose | 600 mg [2] |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a601068 |
| Legal | |
| License data |
|
| Legal status | |
Carbidopa/levodopa, also known as levocarb and co-careldopa, is the combination of the two medications carbidopa and levodopa.[1] It is primarily used to manage the symptoms of Parkinson's disease, but it does not slow down the disease or stop it from getting worse.[1] It is taken by mouth.[1] It can take two to three weeks of treatment before benefits are seen.[3] Each dose then begins working in about ten minutes to two hours with a duration of effect of about five hours.[3][4][5]
Common side effects include movement problems and nausea.[1] More serious side effects include depression, low blood pressure with standing, sudden onset of sleepiness, psychosis, and increased risk-taking behavior.[1][6] Carbidopa prevents the breakdown of levodopa outside the brain.[6] In the brain, levodopa is broken down into dopamine by which it has its effects.[6] Carbidopa also helps prevent some of the nausea which levodopa causes.[7]
It is on the World Health Organization's List of Essential Medicines.[8] It is available as a generic medication and is moderately expensive.[6] The wholesale price in the developing world is about US$1.80 to $3.00 a month.[9] In the United States, a month's supply costs about $50 to $150.[1] In 2020, it was the 364th most commonly prescribed medication in the United States, with more than half a million prescriptions.[10][11]
Medical uses
Parkinson's disease
It is primarily used to improve the symptoms of Parkinson's disease but does not change the course of the disease.[1] It can take two to three weeks of treatment before benefits are seen.[3] Each dose then begins working in about ten minutes to two hours depending on the formulation, with a duration of effect of about five hours.[3][4][5]
A formulation that can be given in an intra-intestinal pump, known as Duodopa, is being developed.[12][13]
Other
Other uses include for dopamine-responsive dystonia (DRD) and restless legs syndrome.[6]
There is tentative evidence that it is useful in amblyopia when used with other treatments.[14]
Dosage
The defined daily dose is 600 mg (by mouth).[2] The initial dose of the normal release medication is generally 100 mg of levodopa with 25 mg of carbidopa three times per day.[1] This is than increased every day or two by 100mg/25mg until 800 mg / 200 mg is achieved or side effects occur.[1] Smaller doses should be used in older people.[15]
Side effects
Common side effects include movement problems, and nausea.[1] Most common early side effect is hallucinations, as movement problems manifest 5–10 years after initiation of treatment. More serious side effects include depression, low blood pressure with standing, sudden onset of sleepiness, and the compulsion to gamble, engage in sexual behavior, or other risk-taking behavior.[1]
Pregnancy and breastfeeding
Use in pregnancy or breastfeeding is not recommended.[15]
Mechanism of action
Levodopa is converted to dopamine via the action of a naturally occurring enzyme called DOPA decarboxylase. This occurs both in the peripheral circulation and in the central nervous system after levodopa has crossed the blood brain barrier. Activation of central dopamine receptors improves the symptoms of Parkinson's disease; however, activation of peripheral dopamine receptors causes nausea and vomiting. For this reason levodopa is usually administered in combination with a DOPA decarboxylase inhibitor (DDCI), in this case carbidopa, which is very polar (and charged at physiologic pH) and cannot cross the blood brain barrier, however prevents peripheral conversion of levodopa to dopamine and thereby reduces the unwanted peripheral side effects of levodopa. Use of carbidopa also increases the quantity of levodopa in the bloodstream that is available to enter the brain.
History
In 1960 the Austrian biochemist Oleh Hornykiewicz, while at the University of Vienna, examined results of autopsies of patients who had died with Parkinson's disease. He suggested that the disease was associated with, or caused by, a reduction in the levels of dopamine in the basal ganglia of the brain. Since dopamine itself did not enter the brain, he tried treating twenty patients with a racemic mixture of dihydroxyphenylalanine (DOPA), which could enter the brain and be converted there to dopamine by the action of DOPA decarboxylase. His results were positive, as were those of another trial in Montreal run by André Barbeau. Unfortunately, other investigators were unable to replicate these early results, and the use of DOPA remained in question until 1967, when George Cotzias at the Brookhaven National Laboratories in Upton, New York, used megadoses of DOPA, up to 16 grams per day. Not long after these results became known, Curt Porter at Merck showed that L-DOPA was the active stereoisomer, thus reducing the effective dose to half.[16]
With L-DOPA identified as the active form, Alfred Pletscher and his colleagues at Hoffman-LaRoche synthesized benserazide, an inhibitor of DOPA decarboxylase, which further reduced the required dose. A drug combining L-DOPA with benserazide was marketed under the brand name of Madopar. Independent work was carried out by Victor Lotti at Merck in West Point, Pennsylvania. Merck had already synthesized and patented carbidopa, another dopa decarboxylase inhibitor in 1962, and in 1971 Lotti showed that the use of the L-form of carbidopa, further reduced the therapeutic dose of L-DOPA. The combination of L-carbidopa and L-DOPA was marketed under the brand name of Sinemet.[16]
Society and culture
Cost
It is available as a generic medication and is moderately expensive.[6] Globally, the wholesale price of the medication is about US$1.80 to $3.00 a month.[9] In the United States a month's supply is about $50 to $150.[1]
.svg.png.webp) CarbidopaLevodopa costs (US)
CarbidopaLevodopa costs (US).svg.png.webp) CarbidopaLevodopa prescriptions (US)
CarbidopaLevodopa prescriptions (US)
Names
The generic name under the BAN system is Co-careldopa.
It is sold under several brand names, including Sinemet (Merck Sharp & Dohme Limited), Pharmacopa, Atamet, Apo-Levocarb, Duodopa, Kinson, and Pharmacopa, among others.
Extended-release formulations are sold as Rytary and Sinemet-CR. An extended-release enteral solution is sold as Duopa.
Shortages
In 1991, Merck licensed the rights to the manufacture and sale of Sinemet to a newly created joint venture, DuPont Merck Pharmaceutical Company. That same year, approvals for a sustained release formulation (Sinemet CR) which could be taken less frequently were also obtained.[17] DuPont purchased Merck's share in the joint venture in 1998 and began operating the company as DuPont Pharmaceuticals (DuPont Pharma), but Merck continued to manufacture the drug for DuPont.[18] Starting in late 2009 and continuing into 2011 Merck stopped manufacturing the drug while awaiting regulatory approvals due to a change in the supplier of the active ingredient. This resulted in shortages of the brand name products Sinemet and Sinemet CR, although alternative generic versions were still available.[19]
Another shortage appears to have occurred at the end of 2017.[20][21]
See also
- Stalevo in combination with entacapone
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 "Levodopa/Carbidopa". The American Society of Health-System Pharmacists. Archived from the original on 24 September 2015. Retrieved 21 August 2015.
- 1 2 "WHOCC - ATC/DDD Index". www.whocc.no. Archived from the original on 23 October 2020. Retrieved 22 September 2020.
- 1 2 3 4 Pharmacology and the Nursing Process. Elsevier Health Sciences. 2014. p. 246. ISBN 9780323293617. Archived from the original on 5 July 2017.
- 1 2 Atlee, John L. (2007). Complications in anesthesia (2nd ed.). Philadelphia: Elsevier/Saunders. p. 490. ISBN 9781416022152. Archived from the original on 15 March 2017.
- 1 2 The new Parkinson's disease treatment book : partnering with your doctor to get the most from your medications (2 ed.). Oxford University Press. 2015. p. 227. ISBN 9780190231866. Archived from the original on 29 August 2021. Retrieved 21 August 2019.
- 1 2 3 4 5 6 Hamilton, Richard J. (2013). Tarascon pocket pharmacopoeia (14th ed.). Burlington, MA.: Jones & Bartlett Learning. p. 303. ISBN 9781449673635. Archived from the original on 12 January 2016.
- ↑ Ahlskog, J. Eric (2009). Parkinson's Disease Treatment Guide for Physicians. Oxford University Press. p. 124. ISBN 978-0-19-537177-2. Archived from the original on 29 August 2021. Retrieved 27 December 2019.
- ↑ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- 1 2 "Levodopa + Carbidopa". International Drug Price Indicator Guide. Archived from the original on 12 January 2016. Retrieved 22 August 2015.
- ↑ "The Top 300 of 2020". ClinCalc. Archived from the original on 12 February 2021. Retrieved 7 October 2022.
- ↑ "Carbidopa; Levodopa - Drug Usage Statistics". ClinCalc. Archived from the original on 8 July 2020. Retrieved 7 October 2022.
- ↑ "Fact sheet - Duodopa (levodopa/carbidopa intestinal gel)". Hc-sc.gc.ca. 11 August 2010. Archived from the original on 11 January 2013. Retrieved 5 February 2013.
- ↑ "Abbott Healthcare - Information on Duodopa". Duodopa.co.uk. Archived from the original on 1 January 2013. Retrieved 5 February 2013.
- ↑ DeSantis, D (June 2014). "Amblyopia". Pediatric Clinics of North America. 61 (3): 505–18. doi:10.1016/j.pcl.2014.03.006. PMID 24852148.
- 1 2 "LEVODOPA/CARBIDOPA oral - Essential drugs". medicalguidelines.msf.org. Archived from the original on 10 May 2021. Retrieved 31 August 2020.
- 1 2 Scriabine, Alexander (1999). "Discovery and Development of Major Drugs Currently in Use", pp. 222–223 in Pharmaceutical Innovation: Revolutionizing Human Health, edited by Ralph Landau, Basil Achilladelis, and Alexander Scriabine. Philadelphia: Chemical Heritage Press. ISBN 978-0-941901-21-5.
- ↑ Sinemet Archived 11 May 2011 at the Wayback Machine at Dupont Heritage.
- ↑ SINEMET at listingdrugs.com Archived 3 May 2012 at the Wayback Machine
- ↑ Letter From MERCK About SINEMET Shortage Archived 3 July 2011 at the Wayback Machine at Bibmomma's Blog – Reflections of an early onset Parkinson's patient.
- ↑ "FDA Drug Shortages". www.accessdata.fda.gov. Archived from the original on 28 August 2021. Retrieved 16 September 2018.
- ↑ "ASHP - 500 Error". www.ashp.org. Archived from the original on 18 May 2021. Retrieved 27 January 2018.
External links
| Identifiers: |
|---|
- "Carbidopa mixture with levodopa". Drug Information Portal. U.S. National Library of Medicine. Archived from the original on 13 July 2020. Retrieved 12 July 2020.