Medroxyprogesterone acetate
Medroxyprogesterone acetate (MPA), also known as depot medroxyprogesterone acetate (DMPA) in injectable form and sold under the brand name Depo-Provera among others, is a hormonal medication of the progestin type.[9][3] It is used as a method of birth control and as a part of menopausal hormone therapy.[9][3] It is also used to treat endometriosis, abnormal uterine bleeding, abnormal sexuality in males, and certain types of cancer.[9] The medication is available both alone and in combination with an estrogen.[10][11] It is taken by mouth, used under the tongue, or by injection into a muscle or fat.[9]
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /mɛˌdrɒksiproʊˈdʒɛstəroʊn ˈæsɪteɪt/ me-DROKS-ee-proh-JES-tər-ohn ASS-i-tayt[1] |
| Trade names | Provera, Depo-Provera, Depo-SubQ Provera 104, Curretab, Cycrin, Farlutal, Gestapuran, Perlutex, Veramix, others[2] |
| Other names | MPA; DMPA; Methylhydroxy |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a604039 |
| Routes of administration | By mouth, sublingual, intramuscular injection, subcutaneous injection |
| Drug class | Progestogen; Progestin; Progestogen ester; Antigonadotropin; Steroidal antiandrogen |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | By mouth: ~100%[3][4] |
| Protein binding | 88% (to albumin)[4] |
| Metabolism | Liver (hydroxylation (CYP3A4), reduction, conjugation)[5][3][6] |
| Elimination half-life | By mouth: 12–33 hours[5][3] IM (aq. susp.): ~50 days[7] SC (aq. susp.): ~40 days[8] |
| Excretion | Urine (as conjugates)[5] |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.689 |
| Chemical and physical data | |
| Formula | C24H34O4 |
| Molar mass | 386.532 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 207 to 209 °C (405 to 408 °F) |
SMILES
| |
InChI
| |
| (verify) | |
Common side effects include menstrual disturbances such as absence of periods, abdominal pain, and headaches.[9] More serious side effects include bone loss, blood clots, allergic reactions, and liver problems.[9] Use is not recommended during pregnancy as it may harm the baby.[9] MPA is an artificial progestogen, and as such activates the progesterone receptor, the biological target of progesterone.[3] It also has androgenic activity and weak glucocorticoid activity. Due to its progestogenic activity, MPA decreases the body's release of gonadotropins and can suppress sex hormone levels.[12] It works as a form of birth control by preventing ovulation.[9]
MPA was discovered in 1956 and was introduced for medical use in the United States in 1959.[13][14][9] It is on the World Health Organization's List of Essential Medicines.[15] MPA is the most widely used progestin in menopausal hormone therapy and in progestogen-only birth control.[16][17] DMPA is approved for use as a form of long-acting birth control in more than 100 countries.[18][19] In 2020, it was the 214th most commonly prescribed medication in the United States, with more than 2 million prescriptions.[20][21]
Medical uses
The most common use of MPA is in the form of DMPA as a long-acting progestogen-only injectable contraceptive to prevent pregnancy in women. It is an extremely effective contraceptive when used with relatively high doses to prevent ovulation. MPA is also used in combination with an estrogen in menopausal hormone therapy in postmenopausal women to treat and prevent menopausal symptoms such as hot flashes, vaginal atrophy, and osteoporosis.[3] It is used in menopausal hormone therapy specifically to prevent endometrial hyperplasia and cancer that would otherwise be induced by prolonged unopposed estrogen therapy in women with intact uteruses.[3][22] In addition to contraception and menopausal hormone therapy, MPA is used in the treatment of gynecological and menstrual disorders such as dysmenorrhea, amenorrhea, and endometriosis.[23] Along with other progestins, MPA was developed to allow for oral progestogen therapy, as progesterone (the progestogen hormone made by the human body) could not be taken orally for many decades before the process of micronization was developed and became feasible in terms of pharmaceutical manufacturing.[24]
DMPA reduces sex drive in men and is used as a form of chemical castration to control inappropriate or unwanted sexual behavior in those with paraphilias or hypersexuality, including in convicted sex offenders.[25][26] DMPA has also been used to treat benign prostatic hyperplasia, as a palliative appetite stimulant for cancer patients, and at high doses (800 mg per day) to treat certain hormone-dependent cancers including endometrial cancer, renal cancer, and breast cancer.[27][28][29][30][31] MPA has also been prescribed in feminizing hormone therapy for transgender women due to its progestogenic and functional antiandrogenic effects.[32] It has been used to delay puberty in children with precocious puberty but is not satisfactory for this purpose as it is not able to completely suppress puberty.[33] DMPA at high doses has been reported to be definitively effective in the treatment of hirsutism as well.[34]
Though not used as a treatment for epilepsy, MPA has been found to reduce the frequency of seizures and does not interact with antiepileptic medications. MPA does not interfere with blood clotting and appears to improve blood parameters for women with sickle cell anemia. Similarly, MPA does not appear to affect liver metabolism, and may improve primary biliary cirrhosis and chronic active hepatitis. Women taking MPA may experience spotting shortly after starting the medication but is not usually serious enough to require medical intervention. With longer use amenorrhea (absence of menstruation) can occur as can irregular menstruation which is a major source of dissatisfaction, though both can result in improvements with iron deficiency and risk of pelvic inflammatory disease and often do not result in discontinuation of the medication.[28]
Birth control
| Depot medroxyprogesterone acetate (DMPA) | |
|---|---|
 | |
| Background | |
| Type | Hormonal |
| First use | 1969[35] |
| Trade names | Depo-Provera, Depo-SubQ Provera 104, others |
| AHFS/Drugs.com | depo-provera |
| Failure rates (first year) | |
| Perfect use | 0.2%[36] |
| Typical use | 6%[36] |
| Usage | |
| Duration effect | 3 months (12–14 weeks) |
| Reversibility | 3–18 months |
| User reminders | Maximum interval is just under 3 months |
| Clinic review | 12 weeks |
| Advantages and disadvantages | |
| STI protection | No |
| Period disadvantages | Especially in first injection may be frequent spotting |
| Period advantages | Usually no periods from 2nd injection |
| Benefits | Especially good if poor pill compliance. Reduced endometrial cancer risk. |
| Risks | Reduced bone density, which may reverse after discontinuation |
| Medical notes | |
| For those intending to start family, suggest switch 6 months prior to alternative method (e.g. POP) allowing more reliable return fertility. | |
DMPA, under brand names such as Depo-Provera and Depo-SubQ Provera 104, is used in hormonal birth control as a long-lasting progestogen-only injectable contraceptive to prevent pregnancy in women.[37][38] It is given by intramuscular or subcutaneous injection and forms a long-lasting depot, from which it is slowly released over a period of several months. It takes one week to take effect if given after the first five days of the period cycle, and is effective immediately if given during the first five days of the period cycle. Estimates of first-year failure rates are about 0.3%.[39] MPA is effective in preventing pregnancy, but offers no protection against sexually transmitted infections (STIs).
Effectiveness
Trussell's estimated perfect use first-year failure rate for DMPA as the average of failure rates in seven clinical trials at 0.3%.[39][40] It was considered perfect use because the clinical trials measured efficacy during actual use of DMPA defined as being no longer than 14 or 15 weeks after an injection (i.e., no more than 1 or 2 weeks late for a next injection).
Prior to 2004, Trussell's typical use failure rate for DMPA was the same as his perfect use failure rate: 0.3%.[41]
- DMPA estimated typical use first-year failure rate = 0.3% in:
In 2004, using the 1995 NSFG failure rate, Trussell increased (by 10 times) his typical use failure rate for DMPA from 0.3% to 3%.[39][40]
- DMPA estimated typical use first-year failure rate = 3% in:
Trussell did not use 1995 NSFG failure rates as typical use failure rates for the other two then newly available long-acting contraceptives, the Norplant implant (2.3%) and the ParaGard copper T 380A IUD (3.7%), which were (as with DMPA) an order of magnitude higher than in clinical trials. Since Norplant and ParaGard allow no scope for user error, their much higher 1995 NSFG failure rates were attributed by Trussell to contraceptive overreporting at the time of a conception leading to a live birth.[39][46][40]
Advantages
DMPA has a number of advantages and benefits:[47][48][38][49]
- Highly effective at preventing pregnancy.
- Injected every 12 weeks. The only continuing action is to book subsequent follow-up injections every twelve weeks, and to monitor side effects to ensure that they do not require medical attention.
- No estrogen. No increased risk of deep vein thrombosis, pulmonary embolism, stroke, or myocardial infarction.
- Minimal drug interactions (compared to other hormonal contraceptives).
- Decreased risk of endometrial cancer. DMPA reduces the risk of endometrial cancer by 80%.[50][51][52] The reduced risk of endometrial cancer in DMPA users is thought to be due to both the direct anti-proliferative effect of progestogen on the endometrium and the indirect reduction of estrogen levels by suppression of ovarian follicular development.[53]
- Decreased risk of iron deficiency anemia, pelvic inflammatory disease (PID), ectopic pregnancy,[54][55] and uterine fibroids.
- Decreased symptoms of endometriosis.
- Decreased incidence of primary dysmenorrhea, ovulation pain, and functional ovarian cysts.
- Decreased incidence of seizures in women with epilepsy. Additionally, unlike most other hormonal contraceptives, DMPA's contraceptive effectiveness is not affected by enzyme-inducing antiepileptic drugs.[56]
- Decreased incidence and severity of sickle cell crises in women with sickle-cell disease.[38]
The United Kingdom Department of Health has actively promoted Long Acting Reversible Contraceptive use since 2008, particularly for young people;[57] following on from the October 2005 National Institute for Health and Clinical Excellence guidelines.[58] Giving advice on these methods of contraception has been included in the 2009 Quality and Outcomes Framework "good practice" for primary care.[59]
Comparison
Proponents of bioidentical hormone therapy believe that progesterone offers fewer side effects and improved quality of life compared to MPA.[60] The evidence for this view has been questioned; MPA is better absorbed when taken by mouth, with a much longer elimination half-life leading to more stable blood levels[61] though it may lead to greater breast tenderness and more sporadic vaginal bleeding.[60] The two compounds do not differentiate in their ability to suppress endometrial hyperplasia,[60] nor does either increase the risk of pulmonary embolism.[62] The two medications have not been adequately compared in direct tests to clear conclusions about safety and superiority.[24]
Available forms
MPA is available alone in the form of 2.5, 5, and 10 mg oral tablets, as a 150 mg/mL (1 mL) or 400 mg/mL (2.5 mL) microcrystalline aqueous suspension for intramuscular injection, and as a 104 mg (0.65 mL of 160 mg/mL) microcrystalline aqueous suspension for subcutaneous injection.[63][64] It has also been marketed in the form of 100, 200, 250, 400, and 500 mg oral tablets; 500 and 1,000 mg oral suspensions; and as a 50 mg/mL microcrystalline aqueous suspension for intramuscular injection.[65][66] A 100 mg/mL microcrystalline aqueous suspension for intramuscular injection was previously available as well.[63] In addition to single-drug formulations, MPA is available in the form of oral tablets in combination with conjugated estrogens (CEEs), estradiol, and estradiol valerate for use in menopausal hormone therapy, and is available in combination with estradiol cypionate in a microcrystalline aqueous suspension as a combined injectable contraceptive.[10][11][63][18]
Depo-Provera is the brand name for a 150 mg microcrystalline aqueous suspension of DMPA that is administered by intramuscular injection. The shot must be injected into thigh, buttock, or deltoid muscle four times a year (every 11 to 13 weeks), and provides pregnancy protection instantaneously after the first injection.[67] Depo-subQ Provera 104 is a variation of the original intramuscular DMPA that is instead a 104 mg microcrystalline dose in aqueous suspension administered by subcutaneous injection. It contains 69% of the MPA found in the original intramuscular DMPA formulation. It can be injected using a smaller injection needle inserting the medication just below the skin, instead of into the muscle, in either the abdomen or thigh. This subcutaneous injection claims to reduce the side effects of DMPA while still maintaining all the same benefits of the original intramuscular DMPA.
Contraindications
MPA is not usually recommended because of unacceptable health risk or because it is not indicated in the following cases:[68][69]
Conditions where the theoretical or proven risks usually outweigh the advantages of using DMPA:
- Multiple risk factors for arterial cardiovascular disease
- Current deep vein thrombosis or pulmonary embolus
- Migraine headache with aura while using DMPA
- Before evaluation of unexplained vaginal bleeding suspected of being a serious condition
- A history of breast cancer and no evidence of current disease for five years
- Active liver disease: (acute viral hepatitis, severe decompensated cirrhosis, benign or malignant liver tumours)
- Conditions of concern for estrogen deficiency and reduced HDL levels theoretically increasing cardiovascular risk:
- Hypertension with vascular disease
- Current and history of ischemic heart disease
- History of stroke
- Diabetes for over 20 years or with nephropathy/retinopathy/neuropathy or vascular disease
Conditions which represent an unacceptable health risk if DMPA is used:
- Current or recent breast cancer (a hormonally sensitive tumour)
Conditions where use is not indicated and should not be initiated:
MPA is not recommended for use prior to menarche or before or during recovery from surgery.[70]
Side effects
In women, the most common adverse effects of MPA are acne, changes in menstrual flow, drowsiness, and can cause birth defects if taken by pregnant women. Other common side effects include breast tenderness, increased facial hair, decreased scalp hair, difficulty falling or remaining asleep, stomach pain, and weight loss or gain.[23] Lowered libido has been reported as a side effect of MPA in women.[71] DMPA can affect menstrual bleeding. After a year of use, 55% of women experience amenorrhea (missed periods); after two years, the rate rises to 68%. In the first months of use "irregular or unpredictable bleeding or spotting, or, rarely, heavy or continuous bleeding" was reported.[72] MPA does not appear to be associated with vitamin B12 deficiency.[73] Data on weight gain with DMPA likewise are inconsistent.[74][75]
At high doses for the treatment of breast cancer, MPA can cause weight gain and can worsen diabetes mellitus and edema (particularly of the face). Adverse effects peak at five weeks, and are reduced with lower doses. Less frequent effects may include thrombosis (though it is not clear if this is truly a risk, it cannot be ruled out), painful urination, headache, nausea, and vomiting. When used as a form of androgen deprivation therapy in men, more frequent complaints include reduced libido, impotence, reduced ejaculate volume, and within three days, chemical castration. At extremely high doses (used to treat cancer, not for contraception) MPA may cause adrenal suppression and may interfere with carbohydrate metabolism, but does not cause diabetes.[28]
When used as a form of injected birth control, there is a delayed return of fertility. The average return to fertility is 9 to 10 months after the last injection, taking longer for overweight or obese women. By 18 months after the last injection, fertility is the same as that in former users of other contraceptive methods.[47][48] Fetuses exposed to progestogens have demonstrated higher rates of genital abnormalities, low birth weight, and increased ectopic pregnancy particularly when MPA is used as an injected form of long-term birth control. A study of accidental pregnancies among poor women in Thailand found that infants who had been exposed to DMPA during pregnancy had a higher risk of low birth weight and an 80% greater-than-usual chance of dying in the first year of life.[76]
Mood changes
There have been concerns about a possible risk of depression and mood changes with progestins like MPA, and this has led to reluctance of some clinicians and women to use them.[77][78] However, contrary to widely-held beliefs, most research suggests that progestins do not cause adverse psychological effects such as depression or anxiety.[77] A 2018 systematic review of the relationship between progestin-based contraception and depression included three large studies of DMPA and reported no association between DMPA and depression.[79] According to a 2003 review of DMPA, the majority of published clinical studies indicate that DMPA is not associated with depression, and the overall data support the notion that the medication does not significantly affect mood.[80]
In the largest study to have assessed the relationship between MPA and depression to date, in which over 3,900 women were treated with DMPA for up to 7 years, the incidence of depression was infrequent at 1.5% and the discontinuation rate due to depression was 0.5%.[79][37][81] This study did not include baseline data on depression,[81] and due to the incidence of depression in the study, the FDA required package labeling for DMPA stating that women with depression should be observed carefully and that DMPA should be discontinued if depression recurs.[79] A subsequent study of 495 women treated with DMPA over the course of 1 year found that the mean depression score slightly decreased in the whole group of continuing users from 7.4 to 6.7 (by 9.5%) and decreased in the quintile of that group with the highest depression scores at baseline from 15.4 to 9.5 (by 38%).[81] Based on the results of this study and others, a consensus began emerging that DMPA does not in fact increase the risk of depression nor worsen the severity of pre-existing depression.[75][81][37]
Similarly to the case of DMPA for hormonal contraception, the Heart and Estrogen/Progestin Replacement Study (HERS), a study of 2,763 postmenopausal women treated with 0.625 mg/day oral CEEs plus 2.5 mg/day oral MPA or placebo for 36 months as a method of menopausal hormone therapy, found no change in depressive symptoms.[82][83][84] However, some small studies have reported that progestins like MPA might counteract beneficial effects of estrogens against depression.[77][3][85]
Long-term effects
The Women's Health Initiative investigated the use of a combination of oral CEEs and MPA compared to placebo. The study was prematurely terminated when previously unexpected risks were discovered, specifically the finding that though the all-cause mortality was not affected by the hormone therapy, the benefits of menopausal hormone therapy (reduced risk of hip fracture, colorectal and endometrial cancer and all other causes of death) were offset by increased risk of coronary heart disease, breast cancer, strokes and pulmonary embolism.[86]
When combined with CEEs, MPA has been associated with an increased risk of breast cancer, dementia, and thrombus in the eye. In combination with estrogens in general, MPA may increase the risk of cardiovascular disease, with a stronger association when used by postmenopausal women also taking CEEs. It was because of these unexpected interactions that the Women's Health Initiative study was ended early due to the extra risks of menopausal hormone therapy,[87] resulting in a dramatic decrease in both new and renewal prescriptions for hormone therapy.[88]
Long-term studies of users of DMPA have found slight or no increased overall risk of breast cancer. However, the study population did show a slightly increased risk of breast cancer in recent users (DMPA use in the last four years) under age 35, similar to that seen with the use of combined oral contraceptive pills.[72]
| Clinical outcome | Hypothesized effect on risk |
Estrogen and progestogen (CEs 0.625 mg/day p.o. + MPA 2.5 mg/day p.o.) (n = 16,608, with uterus, 5.2–5.6 years follow up) |
Estrogen alone (CEs 0.625 mg/day p.o.) (n = 10,739, no uterus, 6.8–7.1 years follow up) | ||||
|---|---|---|---|---|---|---|---|
| HR | 95% CI | AR | HR | 95% CI | AR | ||
| Coronary heart disease | Decreased | 1.24 | 1.00–1.54 | +6 / 10,000 PYs | 0.95 | 0.79–1.15 | −3 / 10,000 PYs |
| Stroke | Decreased | 1.31 | 1.02–1.68 | +8 / 10,000 PYs | 1.37 | 1.09–1.73 | +12 / 10,000 PYs |
| Pulmonary embolism | Increased | 2.13 | 1.45–3.11 | +10 / 10,000 PYs | 1.37 | 0.90–2.07 | +4 / 10,000 PYs |
| Venous thromboembolism | Increased | 2.06 | 1.57–2.70 | +18 / 10,000 PYs | 1.32 | 0.99–1.75 | +8 / 10,000 PYs |
| Breast cancer | Increased | 1.24 | 1.02–1.50 | +8 / 10,000 PYs | 0.80 | 0.62–1.04 | −6 / 10,000 PYs |
| Colorectal cancer | Decreased | 0.56 | 0.38–0.81 | −7 / 10,000 PYs | 1.08 | 0.75–1.55 | +1 / 10,000 PYs |
| Endometrial cancer | – | 0.81 | 0.48–1.36 | −1 / 10,000 PYs | – | – | – |
| Hip fractures | Decreased | 0.67 | 0.47–0.96 | −5 / 10,000 PYs | 0.65 | 0.45–0.94 | −7 / 10,000 PYs |
| Total fractures | Decreased | 0.76 | 0.69–0.83 | −47 / 10,000 PYs | 0.71 | 0.64–0.80 | −53 / 10,000 PYs |
| Total mortality | Decreased | 0.98 | 0.82–1.18 | −1 / 10,000 PYs | 1.04 | 0.91–1.12 | +3 / 10,000 PYs |
| Global index | – | 1.15 | 1.03–1.28 | +19 / 10,000 PYs | 1.01 | 1.09–1.12 | +2 / 10,000 PYs |
| Diabetes | – | 0.79 | 0.67–0.93 | 0.88 | 0.77–1.01 | ||
| Gallbladder disease | Increased | 1.59 | 1.28–1.97 | 1.67 | 1.35–2.06 | ||
| Stress incontinence | – | 1.87 | 1.61–2.18 | 2.15 | 1.77–2.82 | ||
| Urge incontinence | – | 1.15 | 0.99–1.34 | 1.32 | 1.10–1.58 | ||
| Peripheral artery disease | – | 0.89 | 0.63–1.25 | 1.32 | 0.99–1.77 | ||
| Probable dementia | Decreased | 2.05 | 1.21–3.48 | 1.49 | 0.83–2.66 | ||
| Abbreviations: CEs = conjugated estrogens. MPA = medroxyprogesterone acetate. p.o. = per oral. HR = hazard ratio. AR = attributable risk. PYs = person–years. CI = confidence interval. Notes: Sample sizes (n) include placebo recipients, which were about half of patients. "Global index" is defined for each woman as the time to earliest diagnosis for coronary heart disease, stroke, pulmonary embolism, breast cancer, colorectal cancer, endometrial cancer (estrogen plus progestogen group only), hip fractures, and death from other causes. Sources: See template. | |||||||
Blood clots
DMPA has been associated in multiple studies with a higher risk of venous thromboembolism (VTE) when used as a form of progestogen-only birth control in premenopausal women.[89][90][91][92] The increase in incidence of VTE ranges from 2.2-fold to 3.6-fold.[89][90][91][92] Elevated risk of VTE with DMPA is unexpected, as DMPA has little or no effect on coagulation and fibrinolytic factors,[93][94] and progestogens by themselves normally do not increase the risk of thrombosis.[90][91] It has been argued that the higher incidence with DMPA has reflected preferential prescription of DMPA to women considered to be at an increased risk of VTE.[90] Alternatively, it is possible that MPA may be an exception among progestins in terms of VTE risk.[95][96][97] A 2018 meta-analysis reported that MPA was associated with a 2.8-fold higher risk of VTE than other progestins.[96] It is possible that the glucocorticoid activity of MPA may increase the risk of VTE.[3][98][97]
Bone density
DMPA may cause reduced bone density in premenopausal women and in men when used without an estrogen, particularly at high doses, though this appears to be reversible to a normal level even after years of use.
On 17 November 2004, the United States Food and Drug Administration put a black box warning on the label, indicating that there were potential adverse effects of loss of bone mineral density.[99][100] While it causes temporary bone loss, most women fully regain their bone density after discontinuing use.[74] The World Health Organization (WHO) recommends that the use not be restricted.[101][102] The American College of Obstetricians and Gynecologists notes that the potential adverse effects on BMD be balanced against the known negative effects of unintended pregnancy using other birth control methods or no method, particularly among adolescents.
Three studies have suggested that bone loss is reversible after the discontinuation of DMPA.[103][104][105] Other studies have suggested that the effect of DMPA use on postmenopausal bone density is minimal,[106] perhaps because DMPA users experience less bone loss at menopause.[107] Use after peak bone mass is associated with increased bone turnover but no decrease in bone mineral density.[108]
The FDA recommends that DMPA not be used for longer than two years, unless there is no viable alternative method of contraception, due to concerns over bone loss.[100] However, a 2008 Committee Opinion from the American Congress of Obstetricians and Gynecologists (ACOG) advises healthcare providers that concerns about bone mineral density loss should neither prevent the prescription of or continuation of DMPA beyond two years of use.[109]
HIV risk
There is uncertainty regarding the risk of HIV acquisition among DMPA users; some observational studies suggest an increased risk of HIV acquisition among women using DMPA, while others do not.[110] The World Health Organization issued statements in February 2012 and July 2014 saying the data did not warrant changing their recommendation of no restriction – Medical Eligibility for Contraception (MEC) category 1 – on the use of DMPA in women at high risk for HIV.[111][112] Two meta-analyses of observational studies in sub-Saharan Africa were published in January 2015.[113] They found a 1.4- to 1.5-fold increase risk of HIV acquisition for DMPA users relative to no hormonal contraceptive use.[114][115] In January 2015, the Faculty of Sexual & Reproductive Healthcare of the Royal College of Obstetricians and Gynaecologists issued a statement reaffirming that there is no reason to advise against use of DMPA in the United Kingdom even for women at 'high risk' of HIV infection.[116] A systematic review and meta-analysis of risk of HIV infection in DMPA users published in fall of 2015 stated that "the epidemiological and biological evidence now make a compelling case that DMPA adds significantly to the risk of male-to-female HIV transmission."[117] In 2019, a randomized controlled trial found no significant association between DMPA use and HIV.[118]
Breastfeeding
MPA may be used by breastfeeding mothers. Heavy bleeding is possible if given in the immediate postpartum time and is best delayed until six weeks after birth. It may be used within five days if not breast feeding. While a study showed "no significant difference in birth weights or incidence of birth defects" and "no significant alternation of immunity to infectious disease caused by breast milk containing DMPA", a subgroup of babies whose mothers started DMPA at two days postpartum had a 75% higher incidence of doctor visits for infectious diseases during their first year of life.[119]
A larger study with longer follow-up concluded that "use of DMPA during pregnancy or breastfeeding does not adversely affect the long-term growth and development of children". This study also noted that "children with DMPA exposure during pregnancy and lactation had an increased risk of suboptimal growth in height," but that "after adjustment for socioeconomic factors by multiple logistic regression, there was no increased risk of impaired growth among the DMPA-exposed children." The study also noted that effects of DMPA exposure on puberty require further study, as so few children over the age of 10 were observed.[120]
Overdose
MPA has been studied at "massive" dosages of up to 5,000 mg per day orally and 2,000 mg per day via intramuscular injection, without major tolerability or safety issues described.[121][122][123] Overdose is not described in the Food and Drug Administration (FDA) product labels for injected MPA (Depo-Provera or Depo-SubQ Provera 104).[7][8] In the FDA product label for oral MPA (Provera), it is stated that overdose of an estrogen and progestin may cause nausea and vomiting, breast tenderness, dizziness, abdominal pain, drowsiness, fatigue, and withdrawal bleeding.[5] According to the label, treatment of overdose should consist of discontinuation of MPA therapy and symptomatic care.[5]
Interactions
MPA increases the risk of breast cancer, dementia, and thrombus when used in combination with CEEs to treat menopausal symptoms.[70] When used as a contraceptive, MPA does not generally interact with other medications. The combination of MPA with aminoglutethimide to treat metastases from breast cancer has been associated with an increase in depression.[28] St John's wort may decrease the effectiveness of MPA as a contraceptive due to acceleration of its metabolism.[70]
Pharmacology
Pharmacodynamics
MPA acts as an agonist of the progesterone, androgen, and glucocorticoid receptors (PR, AR, and GR, respectively),[4] activating these receptors with EC50 values of approximately 0.01 nM, 1 nM, and 10 nM, respectively.[124] It has negligible affinity for the estrogen receptor.[4] The medication has relatively high affinity for the mineralocorticoid receptor, but in spite of this, it has no mineralocorticoid or antimineralocorticoid activity.[3] The intrinsic activities of MPA in activating the PR and the AR have been reported to be at least equivalent to those of progesterone and dihydrotestosterone (DHT), respectively, indicating that it is a full agonist of these receptors.[125][126]
Progestogen | PR | AR | ER | GR | MR |
|---|---|---|---|---|---|
| Progesterone | 50 | 0 | 0 | 10 | 100 |
| Chlormadinone acetate | 67 | 5 | 0 | 8 | 0 |
| Cyproterone acetate | 90 | 6 | 0 | 6 | 8 |
| Medroxyprogesterone acetate | 115 | 5 | 0 | 29 | 160 |
| Megestrol acetate | 65 | 5 | 0 | 30 | 0 |
| Notes: Values are percentages (%). Reference ligands (100%) were promegestone for the PR, metribolone for the AR, estradiol for the ER, dexamethasone for the GR, and aldosterone for the MR. Sources: [3] | |||||
Progestogenic activity
MPA is a potent agonist of the progesterone receptor with similar affinity and efficacy relative to progesterone.[127] While both MPA and its deacetylated analogue medroxyprogesterone bind to and agonize the PR, MPA has approximately 100-fold higher binding affinity and transactivation potency in comparison.[127] As such, unlike MPA, medroxyprogesterone is not used clinically, though it has seen some use in veterinary medicine.[2] The oral dosage of MPA required to inhibit ovulation (i.e., the effective contraceptive dosage) is 10 mg/day, whereas 5 mg/day was not sufficient to inhibit ovulation in all women.[128] In accordance, the dosage of MPA used in oral contraceptives in the past was 10 mg per tablet.[129] For comparison to MPA, the dosage of progesterone required to inhibit ovulation is 300 mg/day, whereas that of the 19-nortestosterone derivatives norethisterone and norethisterone acetate is only 0.4 to 0.5 mg/day.[130]
The mechanism of action of progestogen-only contraceptives like DMPA depends on the progestogen activity and dose. High-dose progestogen-only contraceptives, such as DMPA, inhibit follicular development and prevent ovulation as their primary mechanism of action.[131][132] The progestogen decreases the pulse frequency of gonadotropin-releasing hormone (GnRH) release by the hypothalamus, which decreases the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) by the anterior pituitary. Decreased levels of FSH inhibit follicular development, preventing an increase in estradiol levels. Progestogen negative feedback and the lack of estrogen positive feedback on LH release prevent a LH surge. Inhibition of follicular development and the absence of a LH surge prevent ovulation.[47][48] A secondary mechanism of action of all progestogen-containing contraceptives is inhibition of sperm penetration by changes in the cervical mucus.[133] Inhibition of ovarian function during DMPA use causes the endometrium to become thin and atrophic. These changes in the endometrium could, theoretically, prevent implantation. However, because DMPA is highly effective in inhibiting ovulation and sperm penetration, the possibility of fertilization is negligible. No available data support prevention of implantation as a mechanism of action of DMPA.[133]
| Compound | Ki (nM) | EC50 (nM)a | EC50 (nM)b |
|---|---|---|---|
| Progesterone | 4.3 | 0.9 | 25 |
| Medroxyprogesterone | 241 | 47 | 32 |
| Medroxyprogesterone acetate | 1.2 | 0.6 | 0.15 |
| Footnotes: a = Coactivator recruitment. b = Reporter cell line. Sources: [127] | |||
| Progestogen | OID (mg/day) | TFD (mg/cycle) | TFD (mg/day) | ODP (mg/day) | ECD (mg/day) |
|---|---|---|---|---|---|
| Progesterone | 300 | 4200 | 200–300 | – | 200 |
| Chlormadinone acetate | 1.7 | 20–30 | 10 | 2.0 | 5–10 |
| Cyproterone acetate | 1.0 | 20 | 1.0 | 2.0 | 1.0 |
| Medroxyprogesterone acetate | 10 | 50 | 5–10 | ? | 5.0 |
| Megestrol acetate | ? | 50 | ? | ? | 5.0 |
| Abbreviations: OID = ovulation-inhibiting dosage (without additional estrogen). TFD = endometrial transformation dosage. ODP = oral dosage in commercial contraceptive preparations. ECD = estimated comparable dosage. Sources: [130][98][134] | |||||
| Compound | Form | Dose for specific uses (mg)[lower-alpha 3] | DOA[lower-alpha 4] | |||
|---|---|---|---|---|---|---|
| TFD[lower-alpha 5] | POICD[lower-alpha 6] | CICD[lower-alpha 7] | ||||
| Algestone acetophenide | Oil soln. | - | – | 75–150 | 14–32 d | |
| Gestonorone caproate | Oil soln. | 25–50 | – | – | 8–13 d | |
| Hydroxyprogest. acetate[lower-alpha 8] | Aq. susp. | 350 | – | – | 9–16 d | |
| Hydroxyprogest. caproate | Oil soln. | 250–500[lower-alpha 9] | – | 250–500 | 5–21 d | |
| Medroxyprog. acetate | Aq. susp. | 50–100 | 150 | 25 | 14–50+ d | |
| Megestrol acetate | Aq. susp. | - | – | 25 | >14 d | |
| Norethisterone enanthate | Oil soln. | 100–200 | 200 | 50 | 11–52 d | |
| Progesterone | Oil soln. | 200[lower-alpha 9] | – | – | 2–6 d | |
| Aq. soln. | ? | – | – | 1–2 d | ||
| Aq. susp. | 50–200 | – | – | 7–14 d | ||
|
Notes and sources:
| ||||||
Antigonadotropic and anticorticotropic effects
MPA suppresses the hypothalamic–pituitary–adrenal (HPA) and hypothalamic–pituitary–gonadal (HPG) axes at sufficient dosages, resulting decreased levels of gonadotropins, androgens, estrogens, adrenocorticotropic hormone (ACTH), and cortisol, as well as levels of sex hormone-binding globulin (SHBG).[12] There is evidence that the suppressive effects of MPA on the HPG axis are mediated by activation of both the PR and the AR in the pituitary gland.[155][156] Due to its effects on androgen levels, MPA can produce strong functional antiandrogenic effects, and is used in the treatment of androgen-dependent conditions such as precocious puberty in boys and hypersexuality in men.[157] In addition, since the medication suppresses estrogen levels as well, MPA can produce strong functional antiestrogenic effects similarly, and has been used to treat estrogen-dependent conditions such as precocious puberty in girls and endometriosis in women. Due to low estrogen levels, the use of MPA without an estrogen poses a risk of decreased bone mineral density and other symptoms of estrogen deficiency.[158]
Oral MPA has been found to suppress testosterone levels in men by about 30% (from 831 ng/dL to 585 ng/dL) at a dosage of 20 mg/day, by about 45 to 75% (average 60%; to 150–400 ng/dL) at a dosage of 60 mg/day,[159][160][161] and by about 70 to 75% (from 832–862 ng/dL to 214–251 ng/dL) at a dosage of 100 mg/day.[162][163] Dosages of oral MPA of 2.5 to 30 mg/day in combination with estrogens have been used to help suppress testosterone levels in transgender women.[164][165][166][167][168][169] One study of injectable MPA in men with benign prostatic hyperplasia reported that a single 150 mg dose suppressed testosterone levels into the defined male castrate range (<58 ng/dL) within 7 days and that castration levels of testosterone were maintained for 3 months.[170] Very high doses of intramuscular MPA of 150 to 500 mg per week (but up to 900 mg per week) have similarly been reported to suppress testosterone levels to less than 100 ng/dL.[159][171] The typical initial dose of intramuscular MPA for testosterone suppression in men with paraphilias is 400 or 500 mg per week.[159]
Androgenic activity
MPA is a potent full agonist of the AR. Its activation of the AR may play an important and major role in its antigonadotropic effects and in its beneficial effects against breast cancer.[155][172][173] However, although MPA may produce androgenic side effects such as acne and hirsutism in some women,[174][175]. In fact, likely due to its suppressive actions on androgen levels, it has been reported that MPA is generally highly effective in improving pre-existing symptoms of hirsutism in women with the condition.[176][177] However, MPA has been seen to cause androgenic effects in children with precocious puberty.[178] The reason for the general lack of virilizing effects with MPA, despite it binding to and activating the AR with high affinity and this action potentially playing an important role in many of its physiological and therapeutic effects, is not entirely clear. However, MPA has been found to interact with the AR differently compared to other agonists of the receptor such as dihydrotestosterone (DHT).[125] The result of this difference appears to be that MPA binds to the AR with a similar affinity and intrinsic activity to that of DHT, but requires about 100-fold higher concentrations for a comparable induction of gene transcription, while at the same time not antagonizing the transcriptional activity of normal androgens like DHT at any concentration.[125] Thus, this may explain the low propensity of MPA for producing androgenic side effects.[125]
MPA shows weak androgenic effects on liver protein synthesis, similarly to other weakly androgenic progestins like megestrol acetate and 19-nortestosterone derivatives.[3][6] While it does not antagonize estrogen-induced increases in levels of triglycerides and HDL cholesterol, DMPA every other week may decrease levels of HDL cholesterol.[3] In addition, MPA has been found to suppress sex hormone-binding globulin (SHBG) production by the liver.[6][179][180] At a dosage of 10 mg/day oral MPA, it has been found to decrease circulating SHBG levels by 14 to 18% in women taking 4 mg/day oral estradiol valerate.[6] Conversely, in a study that combined 2.5 mg/day oral MPA with various oral estrogens, no influence of MPA on estrogen-induced increases in SHBG levels was discerned.[180] In another, higher-dose study, SHBG levels were lower by 59% in a group of women treated with 50 mg/day oral MPA alone relative to an untreated control group of women.[179] In massive-dose studies of oral or injectable MPA (e.g., 500–1,000 mg/day), the medication decreased SHBG levels by about 80%.[181][182][183]
Unlike the related steroids megestrol acetate and cyproterone acetate, MPA is not an antagonist of the AR and does not have direct antiandrogenic activity.[3] As such, although MPA is sometimes described as an antiandrogen, it is not a "true" antiandrogen (i.e., AR antagonist).[160]
Glucocorticoid activity
As an agonist of the GR, MPA has glucocorticoid activity, and as a result can cause symptoms of Cushing's syndrome,[184] steroid diabetes, and adrenal insufficiency at sufficiently high doses.[185] It has been suggested that the glucocorticoid activity of MPA may contribute to bone loss.[186] The glucocorticoid activity of MPA may also result in an upregulation of the thrombin receptor in blood vessel walls, which may contribute to procoagulant effects of MPA and risk of venous thromboembolism and atherosclerosis.[3] The relative glucocorticoid activity of MPA is among the highest of the clinically used progestins.[3]
| Steroid | Class | TR (↑)a | GR (%)b |
|---|---|---|---|
| Dexamethasone | Corticosteroid | ++ | 100 |
| Ethinylestradiol | Estrogen | – | 0 |
| Etonogestrel | Progestin | + | 14 |
| Gestodene | Progestin | + | 27 |
| Levonorgestrel | Progestin | – | 1 |
| Medroxyprogesterone acetate | Progestin | + | 29 |
| Norethisterone | Progestin | – | 0 |
| Norgestimate | Progestin | – | 1 |
| Progesterone | Progestogen | + | 10 |
| Footnotes: a = Thrombin receptor (TR) upregulation (↑) in vascular smooth muscle cells (VSMCs). b = RBA (%) for the glucocorticoid receptor (GR). Strength: – = No effect. + = Pronounced effect. ++ = Strong effect. Sources: [187] | |||
Steroidogenesis inhibition
MPA has been found to act as a competitive inhibitor of rat 3α-hydroxysteroid dehydrogenase (3α-HSD).[188][189][190][191] This enzyme is essential for the transformation of progesterone, deoxycorticosterone, and DHT into inhibitory neurosteroids such as allopregnanolone, THDOC, and 3α-androstanediol, respectively.[192] MPA has been described as very potent in its inhibition of rat 3α-HSD, with an IC50 of 0.2 μM and a Ki (in rat testicular homogenates) of 0.42 μM.[188][189] However, inhibition of 3α-HSD by MPA does not appear to have been confirmed using human proteins yet, and the concentrations required with rat proteins are far above typical human therapeutic concentrations.[188][189]
MPA has been identified as a competitive inhibitor of human 3β-hydroxysteroid dehydrogenase/Δ5-4 isomerase II (3β-HSD II).[193] This enzyme is essential for the biosynthesis of sex steroids and corticosteroids.[193] The Ki of MPA for inhibition of 3β-HSD II is 3.0 μM, and this concentration is reportedly near the circulating levels of the medication that are achieved by very high therapeutic dosages of MPA of 5 to 20 mg/kg/day (dosages of 300 to 1,200 mg/day for a 60 kg (132 lb) person).[193] Aside from 3β-HSD II, other human steroidogenic enzymes, including cholesterol side-chain cleavage enzyme (P450scc/CYP11A1) and 17α-hydroxylase/17,20-lyase (CYP17A1), were not found to be inhibited by MPA.[193] MPA has been found to be effective in the treatment of gonadotropin-independent precocious puberty and in breast cancer in postmenopausal women at high dosages, and inhibition of 3β-HSD II could be responsible for its effectiveness in these conditions.[193]
GABAA receptor allosteric modulation
Progesterone, via transformation into neurosteroids such as 5α-dihydroprogesterone, 5β-dihydroprogesterone, allopregnanolone, and pregnanolone (catalyzed by the enzymes 5α- and 5β-reductase and 3α- and 3β-HSD), is a positive allosteric modulator of the GABAA receptor, and is associated with a variety of effects mediated by this property including dizziness, sedation, hypnotic states, mood changes, anxiolysis, and cognitive/memory impairment, as well as effectiveness as an anticonvulsant in the treatment of catamenial epilepsy.[192][194] It has also been found to produce anesthesia via this action in animals when administered at sufficiently high dosages.[194] MPA was found to significantly reduce seizure incidence when added to existing anticonvulsant regimens in 11 of 14 women with uncontrolled epilepsy, and has also been reported to induce anesthesia in animals, raising the possibility that it might modulate the GABAA receptor similarly to progesterone.[195][196]
MPA shares some of the same metabolic routes of progesterone and, analogously, can be transformed into metabolites such as 5α-dihydro-MPA (DHMPA) and 3α,5α-tetrahydro-MPA (THMPA).[195] However, unlike the reduced metabolites of progesterone, DHMPA and THMPA have been found not to modulate the GABAA receptor.[195] Conversely, unlike progesterone, MPA itself actually modulates the GABAA receptor, although notably not at the neurosteroid binding site.[195] However, rather than act as a potentiator of the receptor, MPA appears to act as a negative allosteric modulator.[195] Whereas the reduced metabolites of progesterone enhance binding of the benzodiazepine flunitrazepam to the GABAA receptor in vitro, MPA can partially inhibit the binding of flunitrazepam by up to 40% with half-maximal inhibition at 1 μM.[195] However, the concentrations of MPA required for inhibition are high relative to therapeutic concentrations, and hence, this action is probably of little or no clinical relevance.[195] The lack of potentiation of the GABAA receptor by MPA or its metabolites is surprising in consideration of the apparent anticonvulsant and anesthetic effects of MPA described above, and they remain unexplained.[195]
Clinical studies using massive dosages of up to 5,000 mg/day oral MPA and 2,000 mg/day intramuscular MPA for 30 days in women with advanced breast cancer have reported "no relevant side effects", which suggests that MPA has no meaningful direct action on the GABAA receptor in humans even at extremely high dosages.[121]
Appetite stimulation
Although MPA and the closely related medication megestrol acetate are effective appetite stimulants at very high dosages,[197] the mechanism of action of their beneficial effects on appetite is not entirely clear. However, glucocorticoid, cytokine, and possibly anabolic-related mechanisms are all thought to possibly be involved, and a number of downstream changes have been implicated, including stimulation of the release of neuropeptide Y in the hypothalamus, modulation of calcium channels in the ventromedial hypothalamus, and inhibition of the secretion of proinflammatory cytokines including IL-1α, IL-1β, IL-6, and TNF-α, actions that have all been linked to an increase in appetite.[198]
Other activity
MPA weakly stimulates the proliferation of MCF-7 breast cancer cells in vitro, an action that is independent of the classical PRs and is instead mediated via the progesterone receptor membrane component-1 (PGRMC1).[199] Certain other progestins are also active in this assay, whereas progesterone acts neutrally.[199] It is unclear if these findings may explain the different risks of breast cancer observed with progesterone, dydrogesterone, and other progestins such as medroxyprogesterone acetate and norethisterone in clinical studies.[200]
Absorption
Surprisingly few studies have been conducted on the pharmacokinetics of MPA at postmenopausal replacement dosages.[201][3] The bioavailability of MPA with oral administration is approximately 100%.[3] A single oral dose of 10 mg MPA has been found to result in peak MPA levels of 1.2 to 5.2 ng/mL within 2 hours of administration using radioimmunoassay.[201][202] Following this, levels of MPA decreased to 0.09 to 0.35 ng/mL 12 hours post-administration.[201][202] In another study, peak levels of MPA were 3.4 to 4.4 ng/mL within 1 to 4 hours of administration of 10 mg oral MPA using radioimmunoassay.[201][203] Subsequently, MPA levels fell to 0.3 to 0.6 ng/mL 24 hours after administration.[201][203] In a third study, MPA levels were 4.2 to 4.4 ng/mL after an oral dose of 5 mg MPA and 6.0 ng/mL after an oral dose of 10 mg MPA, both using radioimmunoassay as well.[201][204]
Treatment of postmenopausal women with 2.5 or 5 mg/day MPA in combination with estradiol valerate for two weeks has been found to rapidly increase circulating MPA levels, with steady-state concentrations achieved after three days and peak concentrations occurring 1.5 to 2 hours after ingestion.[3][205] With 2.5 mg/day MPA, levels of the medication were 0.3 ng/mL (0.8 nmol/L) in women under 60 years of age and 0.45 ng/mL (1.2 nmol/L) in women 65 years of age or over, and with 5 mg/day MPA, levels were 0.6 ng/mL (1.6 nmol/L) in women under 60 years of age and in women 65 years of age or over.[3][205] Hence, area-under-curve levels of the medication were 1.6 to 1.8 times higher in those who were 65 years of age or older relative to those who were 60 years of age or younger.[6][205] As such, levels of MPA have been found to vary with age, and MPA may have an increased risk of side effects in elderly postmenopausal women.[6][3][205] This study assessed MPA levels using liquid-chromatography–tandem mass spectrometry (LC–MS/MS), a more accurate method of blood determinations.[205]
Oral MPA tablets can be administered sublingually instead of orally.[206][207][208] Rectal administration of MPA has also been studied.[209]
With intramuscular administration of 150 mg microcrystalline MPA in aqueous suspension, the medication is detectable in the circulation within 30 minutes, serum concentrations vary but generally plateau at 1.0 ng/mL (2.6 nmol/L) for 3 months.[210] Following this, there is a gradual decline in MPA levels, and the medication can be detected in the circulation for as long as 6 to 9 months post-injection.[210] The particle size of MPA crystals significantly influences its rate of absorption into the body from the local tissue depot when used as a microcrystalline aqueous suspension via intramuscular injection.[211][212][213] Smaller crystals dissolve faster and are absorbed more rapidly, resulting in a shorter duration of action.[211][212][213] Particle sizes can differ between different formulations of MPA, potentially influencing clinical efficacy and tolerability.[211][212][213][214]
Distribution
The plasma protein binding of MPA is 88%.[3][6] It is weakly bound to albumin and is not bound to sex hormone-binding globulin or corticosteroid-binding globulin.[3][6]
Metabolism
The elimination half-life of MPA via oral administration has been reported as both 11.6 to 16.6 hours[5] and 33 hours,[3] whereas the elimination half-lives with intramuscular and subcutaneous injection of microcrystalline MPA in aqueous suspension are 50 and 40 days, respectively.[7][8] The metabolism of MPA is mainly via hydroxylation, including at positions C6β, C21, C2β, and C1β, mediated primarily via CYP3A4, but 3- and 5-dihydro and 3,5-tetrahydro metabolites of MPA are also formed.[3][6] Deacetylation of MPA and its metabolites (into, e.g., medroxyprogesterone) has been observed to occur in non-human primate research to a substantial extent as well (30 to 70%).[215] MPA and/or its metabolites are also metabolized via conjugation.[70] The C6α methyl and C17α acetoxy groups of MPA make it more resistant to metabolism and allow for greater bioavailability than oral progesterone.[6]
Elimination
MPA is eliminated 20 to 50% in urine and 5 to 10% in feces following intravenous administration.[216] Less than 3% of a dose is excreted in unconjugated form.[216]
Level–effect relationships
With intramuscular administration, the high levels of MPA in the blood inhibit luteinizing hormone and ovulation for several months, with an accompanying decrease in serum progesterone to below 0.4 ng/mL.[210] Ovulation resumes when once blood levels of MPA fall below 0.1 ng/mL.[210] Serum estradiol remains at approximately 50 pg/mL for approximately four months post-injection (with a range of 10–92 pg/mL after several years of use), rising once MPA levels fall below 0.5 ng/mL.[210]
Hot flashes are rare while MPA is found at significant blood levels in the body, and the vaginal lining remains moist and creased. The endometrium undergoes atrophy, with small, straight glands and a stroma that is decidualized. Cervical mucus remains viscous. Because of its steady blood levels over the long term and multiple effects that prevent fertilization, MPA is a very effective means of birth control.[210]
Time–concentration curves
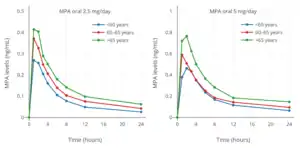 MPA levels with 2.5 or 5 mg/day oral MPA in combination with 1 or 2 mg/day estradiol valerate (Indivina) in postmenopausal women[205]
MPA levels with 2.5 or 5 mg/day oral MPA in combination with 1 or 2 mg/day estradiol valerate (Indivina) in postmenopausal women[205] MPA levels after a single 150 mg intramuscular injection of MPA (Depo-Provera) in aqueous suspension in women[217][218]
MPA levels after a single 150 mg intramuscular injection of MPA (Depo-Provera) in aqueous suspension in women[217][218]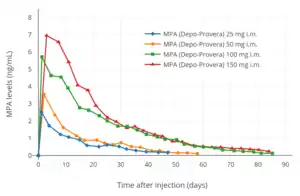 MPA levels after a single 25 to 150 mg intramuscular injection of MPA (Depo-Provera) in aqueous suspension in women[217][219]
MPA levels after a single 25 to 150 mg intramuscular injection of MPA (Depo-Provera) in aqueous suspension in women[217][219]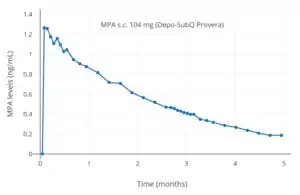 MPA levels after a single 104 mg subcutaneous injection of MPA (Depo-SubQ Provera) in aqueous suspension in women[8]
MPA levels after a single 104 mg subcutaneous injection of MPA (Depo-SubQ Provera) in aqueous suspension in women[8]
Chemistry
MPA is a synthetic pregnane steroid and a derivative of progesterone and 17α-hydroxyprogesterone.[220][2] Specifically, it is the 17α-acetate ester of medroxyprogesterone or the 6α-methylated analogue of hydroxyprogesterone acetate.[220][2] MPA is known chemically as 6α-methyl-17α-acetoxyprogesterone or as 6α-methyl-17α-acetoxypregn-4-ene-3,20-dione, and its generic name is a contraction of 6α-methyl-17α-hydroxyprogesterone acetate.[220][2] MPA is closely related to other 17α-hydroxyprogesterone derivatives such as chlormadinone acetate, cyproterone acetate, and megestrol acetate, as well as to medrogestone and nomegestrol acetate.[220][2] 9α-fluoromedroxyprogesterone acetate (FMPA), the C9α fluoro analogue of MPA and an angiogenesis inhibitor with two orders of magnitude greater potency in comparison to MPA, was investigated for the potential treatment of cancers but was never marketed.[221][222]
History
MPA was independently discovered in 1956 by Syntex and the Upjohn Company.[13][14][223][224] It was first introduced on 18 June 1959 by Upjohn in the United States under the brand name Provera (2.5, 5, and 10 mg tablets) for the treatment of amenorrhea, metrorrhagia, and recurrent miscarriage.[225][226] An intramuscular formulation of MPA, now known as DMPA (400 mg/mL MPA), was also introduced, under the brand name brand name Depo-Provera, in 1960 in the U.S. for the treatment of endometrial and renal cancer.[27] MPA in combination with ethinylestradiol was introduced in 1964 by Upjohn in the U.S. under the brand name Provest (10 mg MPA and 50 μg ethinylestradiol tablets) as an oral contraceptive, but this formulation was discontinued in 1970.[227][228][129] This formulation was marketed by Upjohn outside of the U.S. under the brand names Provestral and Provestrol, while Cyclo-Farlutal (or Ciclofarlutal) and Nogest-S[229] were formulations available outside of the U.S. with a different dosage (5 mg MPA and 50 or 75 μg ethinylestradiol tablets).[230][231]
Following its development in the late 1950s, DMPA was first assessed in clinical trials for use as an injectable contraceptive in 1963.[232] Upjohn sought FDA approval of intramuscular DMPA as a long-acting contraceptive under the brand name Depo-Provera (150 mg/mL MPA) in 1967, but the application was rejected.[233][234] However, this formulation was successfully introduced in countries outside of the United States for the first time in 1969, and was available in over 90 countries worldwide by 1992.[35] Upjohn attempted to gain FDA approval of DMPA as a contraceptive again in 1978, and yet again in 1983, but both applications failed similarly to the 1967 application.[233][234] However, in 1992, the medication was finally approved by the FDA, under the brand name Depo-Provera, for use in contraception.[233] A subcutaneous formulation of DMPA was introduced in the United States as a contraceptive under the brand name Depo-SubQ Provera 104 (104 mg/0.65 mL MPA) in December 2004, and subsequently was also approved for the treatment of endometriosis-related pelvic pain.[235]
MPA has also been marketed widely throughout the world under numerous other brand names such as Farlutal, Perlutex, and Gestapuran, among others.[2][10]
Society and culture
Generic names
Medroxyprogesterone acetate is the generic name of the drug and its INN, USAN, BAN, and JAN, while medrossiprogesterone is the DCIT and médroxyprogestérone the DCF of its free alcohol form.[220][11][2][236][10] It is also known as 6α-methyl-17α-acetoxyprogesterone (MAP) or 6α-methyl-17α-hydroxyprogesterone acetate.[220][11][2][10]
Brand names
MPA is marketed under a large number of brand names throughout the world.[10][11][2] Its most major brand names are Provera as oral tablets and Depo-Provera as an aqueous suspension for intramuscular injection.[10][11][2] A formulation of MPA as an aqueous suspension for subcutaneous injection is also available in the United States under the brand name Depo-SubQ Provera 104.[10][11] Other brand names of MPA formulated alone include Farlutal and Sayana for clinical use and Depo-Promone, Perlutex, Promone-E, and Veramix for veterinary use.[10][11][2] In addition to single-drug formulations, MPA is marketed in combination with the estrogens CEEs, estradiol, and estradiol valerate.[10][11][2] Brand names of MPA in combination with CEEs as oral tablets in different countries include Prempro, Premphase, Premique, Premia, and Premelle.[10][11][2] Brand names of MPA in combination with estradiol as oral tablets include Indivina and Tridestra.[10][11][2]
Availability
Oral MPA and DMPA are widely available throughout the world.[10] Oral MPA is available both alone and in combination with the estrogens CEEs, estradiol, and estradiol valerate.[10] DMPA is registered for use as a form of birth control in more than 100 countries worldwide.[18][19][10] The combination of injected MPA and estradiol cypionate is approved for use as a form of birth control in 18 countries.[18]
United States
As of November 2016, MPA is available in the United States in the following formulations:[63]
- Oral pills: Amen, Curretab, Cycrin, Provera – 2.5 mg, 5 mg, 10 mg
- Aqueous suspension for intramuscular injection: Depo-Provera – 150 mg/mL (for contraception), 400 mg/mL (for cancer)
- Aqueous suspension for subcutaneous injection: Depo-SubQ Provera 104 – 104 mg/0.65 mL (for contraception)
It is also available in combination with an estrogen in the following formulations:
- Oral pills: CEEs and MPA (Prempro, Prempro (Premarin, Cycrin), Premphase (Premarin, Cycrin 14/14), Premphase 14/14, Prempro/Premphase) – 0.3 mg / 1.5 mg; 0.45 mg / 1.5 mg; 0.625 mg / 2.5 mg; 0.625 mg / 5 mg
While the following formulations have been discontinued:
- Oral pills: ethinylestradiol and MPA (Provest) – 50 μg / 10 mg
- Aqueous suspension for intramuscular injection: estradiol cypionate and MPA (Lunelle) – 5 mg / 25 mg (for contraception)
The state of Louisiana permits sex offenders to be given MPA.[237]
Generation
Progestins in birth control pills are sometimes grouped by generation.[238][239] While the 19-nortestosterone progestins are consistently grouped into generations, the pregnane progestins that are or have been used in birth control pills are typically omitted from such classifications or are grouped simply as "miscellaneous" or "pregnanes".[238][239] In any case, based on its date of introduction in such formulations of 1964, MPA could be considered a "first-generation" progestin.[240]
Outside the United States
- In 1994, when DMPA was approved in India, India's Economic and Political Weekly reported that "The FDA finally licensed the drug in 1990 in response to concerns about the population explosion in the third world and the reluctance of third world governments to license a drug not licensed in its originating country."[241] Some scientists and women's groups in India continue to oppose DMPA.[242] In 2016, India introduced DMPA depo-medroxyprogesterone IM preparation in the public health system.[243]
- The Canadian Coalition on Depo-Provera, a coalition of women's health professional and advocacy groups, opposed the approval of DMPA in Canada.[244] Since the approval of DMPA in Canada in 1997, a $700 million class-action lawsuit has been filed against Pfizer by users of DMPA who developed osteoporosis. In response, Pfizer argued that it had met its obligation to disclose and discuss the risks of DMPA with the Canadian medical community.[245]
- Clinical trials for this medication regarding women in Zimbabwe were controversial with regard to human rights abuses and Medical Experimentation in Africa.
- A controversy erupted in Israel when the government was accused of giving DMPA to Ethiopian immigrants without their consent. Some women claimed they were told it was a vaccination. The Israeli government denied the accusations but instructed the four health maintenance organizations to stop administering DMPA injections to women "if there is the slightest doubt that they have not understood the implications of the treatment".[246]
United States
There was a long, controversial history regarding the approval of DMPA by the U.S. Food and Drug Administration. The original manufacturer, Upjohn, applied repeatedly for approval. FDA advisory committees unanimously recommended approval in 1973, 1975 and 1992, as did the FDA's professional medical staff, but the FDA repeatedly denied approval. Ultimately, on 29 October 1992, the FDA approved DMPA for birth control, which had by then been used by over 30 million women since 1969 and was approved and being used by nearly 9 million women in more than 90 countries, including the United Kingdom, France, Germany, Sweden, Thailand, New Zealand and Indonesia.[247] Points in the controversy included:
- Animal testing for carcinogenicity – DMPA caused breast cancer tumors in dogs. Critics of the study claimed that dogs are more sensitive to artificial progesterone, and that the doses were too high to extrapolate to humans. The FDA pointed out that all substances carcinogenic to humans are carcinogenic to animals as well, and that if a substance is not carcinogenic it does not register as a carcinogen at high doses. Levels of DMPA which caused malignant mammary tumors in dogs were equivalent to 25 times the amount of the normal luteal phase progesterone level for dogs. This is lower than the pregnancy level of progesterone for dogs, and is species-specific.[248]
DMPA caused endometrial cancer in monkeys – 2 of 12 monkeys tested, the first ever recorded cases of endometrial cancer in rhesus monkeys.[249] However, subsequent studies have shown that in humans, DMPA reduces the risk of endometrial cancer by approximately 80%.[50][51][52]
Speaking in comparative terms regarding animal studies of carcinogenicity for medications, a member of the FDA's Bureau of Drugs testified at an agency DMPA hearing, "...Animal data for this drug is more worrisome than any other drug we know of that is to be given to well people." - Cervical cancer in Upjohn/NCI studies. Cervical cancer was found to be increased as high as 9-fold in the first human studies recorded by the manufacturer and the National Cancer Institute.[250] However, numerous larger subsequent studies have shown that DMPA use does not increase the risk of cervical cancer.[251][252][253][254][255]
- Coercion and lack of informed consent. Testing or use of DMPA was focused almost exclusively on women in developing countries and poor women in the United States,[256] raising serious questions about coercion and lack of informed consent, particularly for the illiterate[257] and for mentally disabled people, who in some reported cases were given DMPA long-term for reasons of "menstrual hygiene", although they were not sexually active.[258]
- Atlanta/Grady Study – Upjohn studied the effect of DMPA for 11 years in Atlanta, mostly on black women who were receiving public assistance, but did not file any of the required follow-up reports with the FDA. Investigators who eventually visited noted that the studies were disorganized. "They found that data collection was questionable, consent forms and protocol were absent; that those women whose consent had been obtained at all were not told of possible side effects. Women whose known medical conditions indicated that use of DMPA would endanger their health were given the shot. Several of the women in the study died; some of cancer, but some for other reasons, such as suicide due to depression. Over half the 13,000 women in the study were lost to followup due to sloppy record keeping." Consequently, no data from this study was usable.[256]
- WHO Review – In 1992, the WHO presented a review of DMPA in four developing countries to the FDA. The National Women's Health Network and other women's organizations testified at the hearing that the WHO was not objective, as the WHO had already distributed DMPA in developing countries. DMPA was approved for use in United States on the basis of the WHO review of previously submitted evidence from countries such as Thailand, evidence which the FDA had deemed insufficient and too poorly designed for assessment of cancer risk at a prior hearing.
- The Alan Guttmacher Institute has speculated that United States approval of DMPA may increase its availability and acceptability in developing countries.[256][259]
- In 1995, several women's health groups asked the FDA to put a moratorium on DMPA, and to institute standardized informed consent forms.[260]
Research
DMPA was studied by Upjohn for use as a progestogen-only injectable contraceptive in women at a dose of 50 mg once a month but produced poor cycle control and was not marketed for this use at this dosage.[261] A combination of DMPA and polyestradiol phosphate, an estrogen and long-lasting prodrug of estradiol, was studied in women as a combined injectable contraceptive for use by intramuscular injection once every three months.[262][263][264]
High-dose oral and intramuscular MPA monotherapy has been studied in the treatment of prostate cancer but was found to be inferior to monotherapy with cyproterone acetate or diethylstilbestrol.[265][266][267] High-dose oral MPA has been studied in combination with diethylstilbestrol and CEEs as an addition to high-dose estrogen therapy for the treatment of prostate cancer in men, but was not found to provide better effectiveness than diethylstilbestrol alone.[268]
DMPA has been studied for use as a potential male hormonal contraceptive in combination with the androgens/anabolic steroids testosterone and nandrolone (19-nortestosterone) in men.[269] However, it was never approved for this indication.[269]
MPA was investigated by InKine Pharmaceutical, Salix Pharmaceuticals, and the University of Pennsylvania as a potential anti-inflammatory medication for the treatment of autoimmune hemolytic anemia, Crohn's disease, idiopathic thrombocytopenic purpura, and ulcerative colitis, but did not complete clinical development and was never approved for these indications.[270][271] It was formulated as an oral medication at very high dosages, and was thought to inhibit the signaling of proinflammatory cytokines such as interleukin 6 and tumor necrosis factor alpha, with a mechanism of action that was said to be similar to that of corticosteroids.[270][271] The formulation of MPA had the tentative brand names Colirest and Hematrol for these indications.[270]
MPA has been found to be effective in the treatment of manic symptoms in women with bipolar disorder.[272]
Veterinary use
MPA has been used to reduce aggression and spraying in male cats.[273] It may be particularly useful for controlling such behaviors in neutered male cats.[273] The medication can be administered in cats as an injection once per month.[273]
See also
- Conjugated estrogens/medroxyprogesterone acetate
- Estradiol/medroxyprogesterone acetate
- Estradiol cypionate/medroxyprogesterone acetate
- Polyestradiol phosphate/medroxyprogesterone acetate
References
- "Medroxyprogesterone Uses, Dosage & Side Effects".
- Index Nominum 2000: International Drug Directory. Taylor & Francis. January 2000. pp. 638–. ISBN 978-3-88763-075-1. Archived from the original on 19 June 2013.
- Kuhl H (2005). "Pharmacology of estrogens and progestogens: influence of different routes of administration" (PDF). Climacteric. 8 Suppl 1: 3–63. doi:10.1080/13697130500148875. PMID 16112947. S2CID 24616324.
- Schindler AE, Campagnoli C, Druckmann R, Huber J, Pasqualini JR, Schweppe KW, Thijssen JH (2008). "Classification and pharmacology of progestins". Maturitas. 61 (1–2): 171–80. doi:10.1016/j.maturitas.2008.11.013. PMID 19434889.
- "Provera" (PDF). FDA. 2015. Archived from the original (PDF) on 11 February 2017. Retrieved 31 March 2018.
- Stanczyk FZ, Bhavnani BR (September 2015). "Reprint of "Use of medroxyprogesterone acetate for hormone therapy in postmenopausal women: Is it safe?"". J. Steroid Biochem. Mol. Biol. 153: 151–9. doi:10.1016/j.jsbmb.2015.08.013. PMID 26291834. S2CID 23985966.
- "Depo_Provera" (PDF). FDA. 2016. Retrieved 31 March 2018.
- "depo-subQ Provera" (PDF). FDA. 2017. Retrieved 31 March 2018.
- "Medroxyprogesterone Acetate". The American Society of Health-System Pharmacists. Archived from the original on 24 December 2016. Retrieved 8 December 2016.
- "Medroxyprogesterone Uses, Dosage & Side Effects". Drugs.com.
- Sweetman, Sean C., ed. (2009). "Sex hormones and their modulators". Martindale: The Complete Drug Reference (36th ed.). London: Pharmaceutical Press. pp. 2113–2114. ISBN 978-0-85369-840-1.
- Genazzani AR (15 January 1993). Frontiers in Gynecologic and Obstetric Investigation. Taylor & Francis. p. 320. ISBN 978-1-85070-486-7. Archived from the original on 20 May 2016.
- Stanley M. Roberts (7 May 2013). Introduction to Biological and Small Molecule Drug Research and Development: Chapter 12. Hormone replacement therapy. Elsevier Science. pp. 9–. ISBN 978-0-12-806202-9.
[...] medroxyprogesterone acetate, also known as Provera (discovered simultaneously by Searle and Upjohn in 1956) [..]
- Sneader W (2005). "Chapter 18: Hormone analogs". Drug discovery: a history. New York: Wiley. p. 204. ISBN 0-471-89980-1.
- World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- A. Wayne Meikle (1 June 1999). Hormone Replacement Therapy. Springer Science & Business Media. pp. 383–. ISBN 978-1-59259-700-0.
- Special Programme of Research, Development, and Research Training in Human Reproduction (World Health Organization); World Health Organization (2002). Research on Reproductive Health at WHO: Biennial Report 2000-2001. World Health Organization. pp. 17–. ISBN 978-92-4-156208-9.
{{cite book}}: CS1 maint: multiple names: authors list (link) - Bagade O, Pawar V, Patel R, Patel B, Awasarkar V, Diwate S (2014). "Increasing use of long-acting reversible contraception: safe, reliable, and cost-effective birth control" (PDF). World J Pharm Pharm Sci. 3 (10): 364–392. ISSN 2278-4357. Archived from the original (PDF) on 10 August 2017. Retrieved 2 August 2018.
- Sulochana Gunasheela (14 March 2011). Practical Management of Gynecological Problems. JP Medical Ltd. pp. 39–. ISBN 978-93-5025-240-6.
- "The Top 300 of 2020". ClinCalc. Retrieved 7 October 2022.
- "Medroxyprogesterone Acetate - Drug Usage Statistics". ClinCalc. Retrieved 7 October 2022.
- Furness S, Roberts H, Marjoribanks J, Lethaby A (August 2012). "Hormone therapy in postmenopausal women and risk of endometrial hyperplasia". The Cochrane Database of Systematic Reviews (8): CD000402. doi:10.1002/14651858.CD000402.pub4. PMC 7039145. PMID 22895916.
- "Medroxyprogesterone". MedlinePlus. 9 January 2008. Archived from the original on 12 July 2010. Retrieved 2 July 2010.
- Panay N, Fenton A (February 2010). "Bioidentical hormones: what is all the hype about?". Climacteric. 13 (1): 1–3. doi:10.3109/13697130903550250. PMID 20067429. S2CID 244295.
- Light SA, Holroyd S (March 2006). "The use of medroxyprogesterone acetate for the treatment of sexually inappropriate behaviour in patients with dementia" (PDF). Journal of Psychiatry & Neuroscience. 31 (2): 132–4. PMC 1413960. PMID 16575429. Archived (PDF) from the original on 7 March 2016.
- "The chemical knife". Archived from the original on 7 January 2009. Retrieved 22 January 2009.
- Depo-Provera (medroxyprogesterone acetate) (NDA # 012541) - Drugs@FDA: FDA Approved Drug Products, retrieved 2 April 2018,
Original Approvals or Tentative Approvals: 09/23/1960.
- Meyler L (2009). Meyler's side effects of endocrine and metabolic drugs. Amsterdam: Elsevier Science. pp. 281–284]. ISBN 978-0-444-53271-8. Archived from the original on 23 October 2014.
- Ganzina F (October 1979). "High-dose medroxyprogesterone acetate (MPA) treatment in advanced breast cancer. A review". Tumori. 65 (5): 563–85. doi:10.1177/030089167906500507. PMID 390798. S2CID 23378403.
- Kjaer M (September 1988). "The role of medroxyprogesterone acetate (MPA) in the treatment of renal adenocarcinoma". Cancer Treat. Rev. 15 (3): 195–209. doi:10.1016/0305-7372(88)90003-5. PMID 2974757.
- Vanderstappen D, Bonte J (1992). "New trends in the use of medroxyprogesterone acetate as a chemotherapeutic agent in gynecologic malignancies". Eur. J. Gynaecol. Oncol. 13 (2): 113–23. PMID 1534051.
- Gooren L (2005). "Hormone treatment of the adult transsexual patient". Horm. Res. 64 Suppl 2 (2): 31–6. doi:10.1159/000087751. PMID 16286768. S2CID 42507159.
- Anupam Sachdeva; AK Dutta (31 August 2012). Advances in Pediatrics. JP Medical Ltd. pp. 1202–. ISBN 978-93-5025-777-7.
- Hammerstein, J. (1990). "Antiandrogens: Clinical Aspects". Hair and Hair Diseases. pp. 827–886. doi:10.1007/978-3-642-74612-3_35. ISBN 978-3-642-74614-7.
- Anne Nadakavukaren (28 February 2011). Our Global Environment: A Health Perspective, Seventh Edition. Waveland Press. pp. 63–. ISBN 978-1-4786-0976-6.
- Trussell J (2011). "Contraceptive efficacy". In Hatcher RA, Trussell J, Nelson AL, Cates W, Kowal D, Policar MS (eds.). Contraceptive technology (20th revised ed.). New York: Ardent Media. pp. 779–863. ISBN 978-1-59708-004-0. OCLC 781956734. Table 26–1 = Table 3–2 Percentage of women experiencing an unintended pregnancy during the first year of typical use and the first year of perfect use of contraception, and the percentage continuing use at the end of the first year. United States. Archived 15 February 2017 at the Wayback Machine
- Bakry S, Merhi ZO, Scalise TJ, Mahmoud MS, Fadiel A, Naftolin F (July 2008). "Depot-medroxyprogesterone acetate: an update". Arch. Gynecol. Obstet. 278 (1): 1–12. doi:10.1007/s00404-007-0497-z. PMID 18470526. S2CID 11340062.
- Westhoff C (August 2003). "Depot-medroxyprogesterone acetate injection (Depo-Provera): a highly effective contraceptive option with proven long-term safety". Contraception. 68 (2): 75–87. doi:10.1016/S0010-7824(03)00136-7. PMID 12954518.
- Trussell J (2004). "Contraceptive Efficacy". In Hatcher RA, Trussell J, Stewart FH, Nelson AL, Cates Jr W, Guest F, Kowal D (eds.). Contraceptive Technology (18th rev. ed.). New York: Ardent Media. pp. 773–845. ISBN 0-9664902-5-8.
- Trussell J (August 2004). "Contraceptive failure in the United States". Contraception. 70 (2): 89–96. doi:10.1016/j.contraception.2004.03.009. PMC 3638209. PMID 15288211.
- Trussell J, Hatcher RA, Cates W, Stewart FH, Kost K (September 1990). "A guide to interpreting contraceptive efficacy studies". Obstetrics and Gynecology. 76 (3 Pt 2): 558–67. PMID 2199875.
- Trussell J (1994). "Contraceptive Failure Rates". In Hatcher RA, Trussell J, Stewart F, Stewart GK, Kowal D, Guest F, Cates W, Policar MS (eds.). Contraceptive Technology (16th rev. ed.). New York: Irvington Publishers. pp. 637–688. ISBN 0-8290-3171-5.
- Trussell J (1998). "Contraceptive Efficacy". In Hatcher RA, Trussell J, Stewart F, Cates W, Stewart GK, Guest F, Kowal D (eds.). Contraceptive Technology (17th rev. ed.). New York: Ardent Media. pp. 779–844. ISBN 0-9664902-0-7.
- FDA (1998). "Guidance for Industry - Uniform Contraceptive Labeling" (PDF). Food and Drug Administration. Archived from the original (PDF) on 25 February 2007. Retrieved 21 June 2007.
- Trussell J (2007). "Contraceptive Efficacy". In Hatcher RA, Trussell J, Nelson AL, Cates W, Stewart FH, Kowal D (eds.). Contraceptive Technology (19th rev. ed.). New York: Ardent Media. Archived from the original on 31 May 2008. Retrieved 21 June 2007.
- Trussell J, Vaughan B (1999). "Contraceptive failure, method-related discontinuation and resumption of use: results from the 1995 National Survey of Family Growth" (PDF). Family Planning Perspectives. 31 (2): 64–72, 93. doi:10.2307/2991641. JSTOR 2991641. PMID 10224544. Archived (PDF) from the original on 2 December 2008.
- Hatcher RA (2004). "Depo-Provera Injections, Implants, and Progestin-Only Pills (Minipills)". In Hatcher RA, Trussell J, Stewart FH, Nelson AL, Cates Jr W, Guest F, Kowal D (eds.). Contraceptive Technology (18th rev. ed.). New York: Ardent Media. pp. 461–494. ISBN 0-9664902-5-8.
- Speroff L, Darney PD (2005). "Injectable Contraception". A Clinical Guide for Contraception (4th ed.). Philadelphia: Lippincott Williams & Wilkins. pp. 201–220. ISBN 0-7817-6488-2.
- Mishell DR (2004). "Contraception". In Strauss JF, Barbieri RL (eds.). Yen and Jaffe's Reproductive Endocrinology (5th ed.). Philadelphia: Elsevier Saunders. pp. 899–938. ISBN 0-7216-9546-9.
- Kaunitz AM (December 2001). "Current options for injectable contraception in the United States". Seminars in Reproductive Medicine. 19 (4): 331–7. doi:10.1055/s-2001-18641. PMID 11727175.
- Bigrigg A, Evans M, Gbolade B, Newton J, Pollard L, Szarewski A, Thomas C, Walling M (July 1999). "Depo Provera. Position paper on clinical use, effectiveness and side effects". The British Journal of Family Planning. 25 (2): 69–76. PMID 10454658.
- "Depot-medroxyprogesterone acetate (DMPA) and risk of endometrial cancer. The WHO Collaborative Study of Neoplasia and Steroid Contraceptives". International Journal of Cancer. 49 (2): 186–90. September 1991. doi:10.1002/ijc.2910490207. PMID 1831802. S2CID 221776781.
- Santen RJ (2004). "Endocrinology of Breast and Endometrial Cancer". In Strauss JF, Barbieri RL (eds.). Yen and Jaffe's Reproductive Endocrinology (5th ed.). Philadelphia: Elsevier Saunders. pp. 787–809. ISBN 0-7216-9546-9.
- Bartz D, Goldberg AB (2011). "Injectable contraceptives". In Hatcher RA, Trussell J, Nelson AL, Cates W Jr, Kowal D, Policar MS (eds.). Contraceptive technology (20th revised ed.). New York: Ardent Media. pp. 212–213. ISBN 978-1-59708-004-0. OCLC 781956734.
Advantages of DMPA Injectables. 5. Reduced risk of ectopic pregnancy. Compared with women who use no contraceptive at all, women who use DMPA have a reduced risk for having an ectopic pregnancy. Although the overall risk of pregnancy and thus ectopic pregnancy is lowered by DMPA, the possibility of an ectopic pregnancy should be excluded if a woman using DMPA becomes pregnant. One study showed that 1.5% of women who got pregnant on DMPA had an ectopic pregnancy, the same ectopic rate as women who conceived while not using contraception.27
- Borgatta L, Murthy A, Chuang C, Beardsley L, Burnhill MS (September 2002). "Pregnancies diagnosed during Depo-Provera use". Contraception. 66 (3): 169–72. doi:10.1016/S0010-7824(02)00340-2. PMID 12384205.
- O'Brien MD, Guillebaud J (September 2006). "Contraception for women with epilepsy". Epilepsia. 47 (9): 1419–22. doi:10.1111/j.1528-1167.2006.00671.x. PMID 16981856. S2CID 22284176.
- "Increasing use of long-acting reversible contraception". Nursing Times.net. 21 October 2008. Archived from the original on 26 August 2009. Retrieved 19 June 2009.
- "CG30 Long-acting reversible contraception: quick reference guide" (PDF). National Institute for Health and Clinical Excellence. Archived from the original (PDF) on 20 September 2009. Retrieved 19 June 2009.
- "Sexual Health Ruleset" (PDF). New GMS Contract Quality and Outcome Framework - Implementation Dataset and Business Rules. Primary Care Commissioning. 1 May 2009. Archived (PDF) from the original on 10 August 2011. Retrieved 19 June 2009.
Sumarized at
* "Contraception - Management QOF indicators". NHS Clinical Knowledge Summaries. NHS Institute for Innovation and Improvement. Retrieved 19 June 2009. - Holtorf K (January 2009). "The bioidentical hormone debate: are bioidentical hormones (estradiol, estriol, and progesterone) safer or more efficacious than commonly used synthetic versions in hormone replacement therapy?" (PDF). Postgraduate Medicine. 121 (1): 73–85. doi:10.3810/pgm.2009.01.1949. PMID 19179815. S2CID 2060730. Archived from the original (PDF) on 8 July 2011.
- Cirigliano M (June 2007). "Bioidentical hormone therapy: a review of the evidence" (PDF). Journal of Women's Health. 16 (5): 600–31. doi:10.1089/jwh.2006.0311. PMID 17627398. Archived from the original (PDF) on 6 January 2011.
- Boothby LA, Doering PL (August 2008). "Bioidentical hormone therapy: a panacea that lacks supportive evidence". Current Opinion in Obstetrics and Gynecology. 20 (4): 400–7. doi:10.1097/GCO.0b013e3283081ae9. PMID 18660693. S2CID 22449765.
- "Drugs@FDA: FDA Approved Drug Products". United States Food and Drug Administration. Archived from the original on 16 November 2016. Retrieved 31 March 2018.
- Engorn B, Flerlage J (1 May 2014). The Harriet Lane Handbook E-Book. Elsevier Health Sciences. pp. 846–. ISBN 978-0-323-11246-8.
- Adriana P. Tiziani (1 June 2013). Havard's Nursing Guide to Drugs. Elsevier Health Sciences. pp. 989–. ISBN 978-0-7295-8162-2.
- Freimut A. Leidenberger (17 April 2013). Klinische Endokrinologie für Frauenärzte. Springer-Verlag. pp. 528–. ISBN 978-3-662-08110-5.
- Stacey, Dawn. Depo Provera: The Birth Control Shot Archived 10 October 2008 at the Wayback Machine Accessed 13 October 2009.
- WHO (2004). "Progestogen-only contraceptives". Medical Eligibility Criteria for Contraceptive Use (3rd ed.). Geneva: Reproductive Health and Research, WHO. ISBN 92-4-156266-8. Archived from the original on 31 May 2009.
- FFPRHC (2006). "The UK Medical Eligibility Criteria for Contraceptive Use (2005/2006)" (PDF). Archived from the original (PDF) on 19 June 2007. Retrieved 11 January 2007.
- "MedroxyPROGESTERone: Drug Information Provided by Lexi-Comp". Merck Manual. 1 December 2009. Archived from the original on 24 July 2010. Retrieved 8 July 2010.
- King SR (9 November 2012). Neurosteroids and the Nervous System. Springer Science & Business Media. pp. 45–. ISBN 978-1-4614-5559-2. Archived from the original on 5 November 2017.
- Pfizer (October 2004). "Depo-Provera Contraceptive Injection, US patient labeling" (PDF). Archived from the original (PDF) on 6 February 2007. Retrieved 21 February 2007.
- Amatayakul K, Sivasomboon B, Thanangkul O (September 1978). "Vitamin and trace mineral metabolism in medroxyprogesterone acetate users". Contraception. 18 (3): 253–69. doi:10.1016/s0010-7824(78)80019-5. PMID 720068.
- Nelson, Anita L (2014). "DMPA: battered and bruised but still needed and used in the USA". Expert Review of Obstetrics & Gynecology. 5 (6): 673–686. doi:10.1586/eog.10.60. ISSN 1747-4108.
- Jeffrey K. Aronson (15 October 2015). Meyler's Side Effects of Drugs: The International Encyclopedia of Adverse Drug Reactions and Interactions. Elsevier Science. pp. 2–. ISBN 978-0-444-53716-4.
Perhaps surprisingly, a consensus seems to be emerging that depot medroxyprogesterone acetate implants do not in fact result in an increase in the incidence of depression or in the severity of pre-existing depression, even after 1 or 2 years, nor do they cause significant weight gain.
- "Exposure to DMPA in pregnancy may cause low birth weight". Progress in Human Reproduction Research (23): 2–3. 1992. PMID 12286194.
- Rogerio A. Lobo (5 June 2007). Treatment of the Postmenopausal Woman: Basic and Clinical Aspects. Elsevier. pp. 211–. ISBN 978-0-08-055309-2.
- Kaunitz AM (1999). "Long-acting hormonal contraception: assessing impact on bone density, weight, and mood". Int J Fertil Womens Med. 44 (2): 110–7. PMID 10338269.
Despite the efficacy and increasing acceptability of these long-term methods, some clinicians and women are reluctant to use them because of concerns regarding reduction in bone density with DMPA, and depressive symptoms and body weight issues with both injectables and implants. Recent multicenter experience showed no increase in depressive symptoms after 1 year's DMPA use and 2 years' Norplant use, even among users with the highest mean depressive symptom scores pre-therapy.
- Worly BL, Gur TL, Schaffir J (February 2018). "The relationship between progestin hormonal contraception and depression: a systematic review". Contraception. 97 (6): 478–489. doi:10.1016/j.contraception.2018.01.010. PMID 29496297. S2CID 3644828.
- Westhoff C (August 2003). "Depot-medroxyprogesterone acetate injection (Depo-Provera): a highly effective contraceptive option with proven long-term safety". Contraception. 68 (2): 75–87. doi:10.1016/s0010-7824(03)00136-7. PMID 12954518.
Another common patient tolerability concern reported with hormonal contraception is the effect on mood [95]. The majority of published reports indicate that DMPA does not cause depressive symptoms. In a large, 1-year, clinical trial of DMPA in 3857 US women, fewer than 2% of users reported depression [15]. Other reports in various settings, including a private practice [96], adolescent clinics [97,98], a psychiatric hospital [99] and inner-city family-planning clinics [100,101], have not found an adverse effect of DMPA on depression. [...] Using a variety of objective indices for depressive symptoms, the overall data for both OCs and DMPA are supportive that these agents have no significant effect on mood. Although history of mood symptoms prior to OC use may predispose a subgroup of women to negative mood changes, the data for DMPA suggest that even women who have depressive symptoms prior to treatment can tolerate therapy with no exacerbation of these symptoms.
- Westhoff C, Truman C, Kalmuss D, Cushman L, Davidson A, Rulin M, Heartwell S (April 1998). "Depressive symptoms and Depo-Provera". Contraception. 57 (4): 237–40. doi:10.1016/s0010-7824(98)00024-9. PMID 9649914.
- Fink G, Pfaff DW, Levine J (31 August 2011). Handbook of Neuroendocrinology. Academic Press. pp. 564–. ISBN 978-0-12-378554-1.
- Janice Ryden (2009). Practical Gynecology: A Guide for the Primary Care Physician. ACP Press. pp. 379–. ISBN 978-1-934465-05-9.
- Hlatky MA, Boothroyd D, Vittinghoff E, Sharp P, Whooley MA (February 2002). "Quality-of-life and depressive symptoms in postmenopausal women after receiving hormone therapy: results from the Heart and Estrogen/Progestin Replacement Study (HERS) trial". JAMA. 287 (5): 591–7. doi:10.1001/jama.287.5.591. PMID 11829697.
- Wiegratz I, Kuhl H (August 2004). "Progestogen therapies: differences in clinical effects?". Trends Endocrinol. Metab. 15 (6): 277–85. doi:10.1016/j.tem.2004.06.006. PMID 15358281. S2CID 35891204.
- Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA, Howard BV, Johnson KC, Kotchen JM, Ockene J (July 2002). "Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women's Health Initiative randomized controlled trial" (PDF). JAMA. 288 (3): 321–33. doi:10.1001/jama.288.3.321. PMID 12117397. S2CID 20149703.
- Prentice RL, Anderson GL (2008). "The women's health initiative: lessons learned". Annual Review of Public Health. 29: 131–50. doi:10.1146/annurev.publhealth.29.020907.090947. PMID 18348708.
- Buist DS, Newton KM, Miglioretti DL, Beverly K, Connelly MT, Andrade S, Hartsfield CL, Wei F, Chan KA, Kessler L (November 2004). "Hormone therapy prescribing patterns in the United States". Obstetrics and Gynecology. 104 (5 Pt 1): 1042–50. doi:10.1097/01.AOG.0000143826.38439.af. PMID 15516400. S2CID 31593637.
- Beyer-Westendorf J, Bauersachs R, Hach-Wunderle V, Zotz RB, Rott H (October 2018). "Sex hormones and venous thromboembolism - from contraception to hormone replacement therapy". VASA. 47 (6): 441–450. doi:10.1024/0301-1526/a000726. PMID 30008249. S2CID 51628832.
- DeLoughery TG (June 2011). "Estrogen and thrombosis: controversies and common sense". Rev Endocr Metab Disord. 12 (2): 77–84. doi:10.1007/s11154-011-9178-0. PMID 21559819. S2CID 28053690.
- Mantha, S.; Karp, R.; Raghavan, V.; Terrin, N.; Bauer, K. A.; Zwicker, J. I. (2012). "Assessing the risk of venous thromboembolic events in women taking progestin-only contraception: a meta-analysis". BMJ. 345 (aug07 2): e4944. doi:10.1136/bmj.e4944. ISSN 1756-1833. PMC 3413580. PMID 22872710.
- Tepper NK, Jeng G, Curtis KM, Boutot ME, Boulet SL, Whiteman MK (March 2019). "Venous Thromboembolism Among Women Initiating Depot Medroxyprogesterone Acetate Immediately Postpartum". Obstet Gynecol. 133 (3): 533–540. doi:10.1097/AOG.0000000000003135. PMID 30741807.
- Van Hylckama Vlieg, A.; Middeldorp, S. (2011). "Hormone therapies and venous thromboembolism: where are we now?". Journal of Thrombosis and Haemostasis. 9 (2): 257–266. doi:10.1111/j.1538-7836.2010.04148.x. ISSN 1538-7933. PMID 21114755. S2CID 32394836.
- Benagiano, G.; Primiero, F.M. (1983). "Long Acting Contraceptives Present Status". Drugs. 25 (6): 570–609. doi:10.2165/00003495-198325060-00003. ISSN 0012-6667. PMID 6223801. S2CID 45898359.
- Rott H (February 2019). "Birth Control Pills and Thrombotic Risks: Differences of Contraception Methods with and without Estrogen". Hamostaseologie. 39 (1): 42–48. doi:10.1055/s-0039-1677806. PMID 30669160. S2CID 58947063.
- Scarabin PY (August 2018). "Progestogens and venous thromboembolism in menopausal women: an updated oral versus transdermal estrogen meta-analysis". Climacteric. 21 (4): 341–345. doi:10.1080/13697137.2018.1446931. PMID 29570359. S2CID 4229701.
- Sitruk-Ware R, Nath A (June 2011). "Metabolic effects of contraceptive steroids". Rev Endocr Metab Disord. 12 (2): 63–75. doi:10.1007/s11154-011-9182-4. PMID 21538049. S2CID 23760705.
- Kuhl H (2011). "Pharmacology of Progestogens" (PDF). J Reproduktionsmed Endokrinol. 8 (1): 157–177. Archived (PDF) from the original on 11 October 2016.
- "Depot medroxyprogesterone acetate and bone effects. Committee Opinion #602". June 2014. Archived from the original on 30 April 2015. Retrieved 3 May 2015.
- FDA (17 November 2004). "Black Box Warning Added Concerning Long-Term Use of Depo-Provera Contraceptive Injection". Food and Drug Administration. Archived from the original on 21 December 2005. Retrieved 12 May 2006.
- World Health Organization (September 2005). "Hormonal contraception and bone health". Family Planning. Archived from the original on 14 May 2006. Retrieved 12 May 2006.
- Curtis KM, Martins SL (May 2006). "Progestogen-only contraception and bone mineral density: a systematic review". Contraception. 73 (5): 470–87. doi:10.1016/j.contraception.2005.12.010. PMID 16627031.
- Cundy T, Cornish J, Evans MC, Roberts H, Reid IR (January 1994). "Recovery of bone density in women who stop using medroxyprogesterone acetate". BMJ. 308 (6923): 247–8. doi:10.1136/bmj.308.6923.247. PMC 2539337. PMID 8111260.
- Scholes D, LaCroix AZ, Ichikawa LE, Barlow WE, Ott SM (September 2002). "Injectable hormone contraception and bone density: results from a prospective study". Epidemiology. 13 (5): 581–7. doi:10.1097/00001648-200209000-00015. PMID 12192229.
- Scholes D, LaCroix AZ, Ichikawa LE, Barlow WE, Ott SM (February 2005). "Change in bone mineral density among adolescent women using and discontinuing depot medroxyprogesterone acetate contraception". Archives of Pediatrics & Adolescent Medicine. 159 (2): 139–44. doi:10.1001/archpedi.159.2.139. PMID 15699307.
- Orr-Walker BJ, Evans MC, Ames RW, Clearwater JM, Cundy T, Reid IR (November 1998). "The effect of past use of the injectable contraceptive depot medroxyprogesterone acetate on bone mineral density in normal post-menopausal women". Clinical Endocrinology. 49 (5): 615–8. doi:10.1046/j.1365-2265.1998.00582.x. PMID 10197077. S2CID 22565912.
- Cundy T, Cornish J, Roberts H, Reid IR (May 2002). "Menopausal bone loss in long-term users of depot medroxyprogesterone acetate contraception". American Journal of Obstetrics and Gynecology. 186 (5): 978–83. doi:10.1067/mob.2002.122420. PMID 12015524.
- Walsh JS, Eastell R, Peel NF (February 2010). "Depot medroxyprogesterone acetate use after peak bone mass is associated with increased bone turnover but no decrease in bone mineral density". Fertility and Sterility. 93 (3): 697–701. doi:10.1016/j.fertnstert.2008.10.004. PMID 19013564.
- American College of Obstetricians Gynecologists Committee on Gynecologic Practice (September 2008). "ACOG Committee Opinion No. 415: Depot medroxyprogesterone acetate and bone effects". Obstetrics and Gynecology. 112 (3): 727–30. doi:10.1097/AOG.0b013e318188d1ec. PMID 18757687.
- Polis CB, Phillips SJ, Curtis KM, Westreich DJ, Steyn PS, Raymond E, Hannaford P, Turner AN (October 2014). "Hormonal contraceptive methods and risk of HIV acquisition in women: a systematic review of epidemiological evidence". Contraception. 90 (4): 360–90. doi:10.1016/j.contraception.2014.07.009. PMID 25183264.
- WHO Department of Reproductive Health and Research (16 February 2012). "Technical Statement: Hormonal contraception and HIV". Geneva: World Health Organization. Archived from the original on 30 January 2015.
- WHO Department of Reproductive Health and Research (23 July 2014). "2014 Guidance Statement: Hormonal contraceptive methods for women at high risk of HIV and living with HIV" (PDF). Geneva: World Health Organization. Archived from the original (PDF) on 30 January 2015.
- AVAC (27 January 2015). "News from the HC-HIV front: it's raining meta (analyses)!". New York: AIDS Vaccine Advocacy Coalition. Archived from the original on 30 January 2015.
- Ralph LJ, McCoy SI, Shiu K, Padian NS (February 2015). "Hormonal contraceptive use and women's risk of HIV acquisition: a meta-analysis of observational studies". The Lancet. Infectious Diseases. 15 (2): 181–9. doi:10.1016/S1473-3099(14)71052-7. PMC 4526270. PMID 25578825.
- Morrison CS, Chen PL, Kwok C, Baeten JM, Brown J, Crook AM, Van Damme L, Delany-Moretlwe S, Francis SC, Friedland BA, Hayes RJ, Heffron R, Kapiga S, Karim QA, Karpoff S, Kaul R, McClelland RS, McCormack S, McGrath N, Myer L, Rees H, van der Straten A, Watson-Jones D, van de Wijgert JH, Stalter R, Low N (January 2015). "Hormonal contraception and the risk of HIV acquisition: an individual participant data meta-analysis". PLOS Medicine. 12 (1): e1001778. doi:10.1371/journal.pmed.1001778. PMC 4303292. PMID 25612136.
- Faculty of Sexual Reproductive Healthcare (January 2015). "CEU Statement: Depot medroxyprogesterone acetate (DMPA, Depo-Provera) and risk of HIV acquisition" (PDF). London: Royal College of Obstetricians and Gynaecologists. Archived from the original (PDF) on 30 January 2015.
- Brind J, Condly SJ, Mosher SW, Morse AR, Kimball J (2015). "Risk of HIV Infection in Depot-Medroxyprogesterone Acetate (DMPA) Users: A Systematic Review and Meta-analysis". Issues Law Med. 30 (2): 129–39. PMID 26710371.
- ECHO Trial Consortium (13 June 2019). "HIV incidence among women using intramuscular depot medroxyprogesterone acetate, a copper intrauterine device, or a levonorgestrel implant for contraception: a randomised, multicentre, open-label trial". The Lancet. 394 (10195): 303–313. doi:10.1016/S0140-6736(19)31288-7. PMC 6675739. PMID 31204114.
- Dahlberg K (February 1982). "Some effects of depo-medroxyprogesterone acetate (DMPA): observations in the nursing infant and in the long-term user". International Journal of Gynaecology and Obstetrics. 20 (1): 43–8. doi:10.1016/0020-7292(82)90044-3. PMID 6126406. S2CID 8295162.
- Pardthaisong T, Yenchit C, Gray R (April 1992). "The long-term growth and development of children exposed to Depo-Provera during pregnancy or lactation". Contraception. 45 (4): 313–24. doi:10.1016/0010-7824(92)90053-V. PMID 1387602.
- Muss HB, Cruz JM (August 1992). "High-dose progestin therapy for metastatic breast cancer". Annals of Oncology. 3 Suppl 3: 15–20. doi:10.1093/annonc/3.suppl_3.S15. PMID 1390312.
- Pannuti F, Martoni A, Lenaz GR, Piana E, Nanni P (April 1978). "A possible new approach to the treatment of metastatic breast cancer: massive doses of medroxyprogesterone acetate". Cancer Treat Rep. 62 (4): 499–504. PMID 350387.
- Simons JP, Schols AM, Hoefnagels JM, Westerterp KR, ten Velde GP, Wouters EF (February 1998). "Effects of medroxyprogesterone acetate on food intake, body composition, and resting energy expenditure in patients with advanced, nonhormone-sensitive cancer: a randomized, placebo-controlled trial". Cancer. 82 (3): 553–60. doi:10.1002/(sici)1097-0142(19980201)82:3<553::aid-cncr18>3.0.co;2-0. PMID 9452274.
- World Health Organization (2004). Residues of Some Veterinary Drugs in Animals and Food: Monographs Prepared by the Sixty-second Meeting of the Joint FAO/WHO Expert Committee on Food Additives, Rome, 4-12 February 2004. Food & Agriculture Org. p. 49. ISBN 978-92-5-105195-5. Archived from the original on 17 June 2014.
- Kemppainen JA, Langley E, Wong CI, Bobseine K, Kelce WR, Wilson EM (March 1999). "Distinguishing androgen receptor agonists and antagonists: distinct mechanisms of activation by medroxyprogesterone acetate and dihydrotestosterone". Molecular Endocrinology. 13 (3): 440–54. doi:10.1210/mend.13.3.0255. PMID 10077001.
- Bentel JM, Birrell SN, Pickering MA, Holds DJ, Horsfall DJ, Tilley WD (August 1999). "Androgen receptor agonist activity of the synthetic progestin, medroxyprogesterone acetate, in human breast cancer cells". Molecular and Cellular Endocrinology. 154 (1–2): 11–20. doi:10.1016/S0303-7207(99)00109-4. PMID 10509795. S2CID 25584803.
- Pullen MA, Laping N, Edwards R, Bray J (September 2006). "Determination of conformational changes in the progesterone receptor using ELISA-like assays". Steroids. 71 (9): 792–8. doi:10.1016/j.steroids.2006.05.009. PMID 16784762. S2CID 24703323.
- Wikström A, Green B, Johansson ED (1984). "The plasma concentration of medroxyprogesterone acetate and ovarian function during treatment with medroxyprogesterone acetate in 5 and 10 mg doses". Acta Obstetricia et Gynecologica Scandinavica. 63 (2): 163–8. doi:10.3109/00016348409154654. PMID 6233840. S2CID 45767999.
- Blum RW (22 October 2013). Adolescent Health Care: Clinical Issues. Elsevier Science. pp. 216–. ISBN 978-1-4832-7738-7.
- Schindler AE, Campagnoli C, Druckmann R, Huber J, Pasqualini JR, Schweppe KW, Thijssen JH (December 2003). "Classification and pharmacology of progestins". Maturitas. 46 Suppl 1: S7–S16. doi:10.1016/j.maturitas.2003.09.014. PMID 14670641.
- Glasier A (2006). "Contraception". In DeGroot LJ, Jameson JL (eds.). Endocrinology (5th ed.). Philadelphia: Elsevier Saunders. pp. 2993–3003. ISBN 978-0-7216-0376-6.
- Loose DS, Stancel GM (2006). "Estrogens and Progestins". In Brunton LL, Lazo JS, Parker KL (eds.). Goodman & Gilman's The Pharmacological Basis of Therapeutics (11th ed.). New York: McGraw-Hill. pp. 1541–1571. ISBN 0-07-142280-3.
- Rivera R, Yacobson I, Grimes D (November 1999). "The mechanism of action of hormonal contraceptives and intrauterine contraceptive devices". American Journal of Obstetrics and Gynecology. 181 (5 Pt 1): 1263–9. doi:10.1016/S0002-9378(99)70120-1. PMID 10561657.
- Fritz MA, Speroff L (28 March 2012). Clinical Gynecologic Endocrinology and Infertility. Lippincott Williams & Wilkins. pp. 761–. ISBN 978-1-4511-4847-3.
- Knörr K, Beller FK, Lauritzen C (17 April 2013). Lehrbuch der Gynäkologie. Springer-Verlag. pp. 214–. ISBN 978-3-662-00942-0.
- Knörr K, Knörr-Gärtner H, Beller FK, Lauritzen C (8 March 2013). Geburtshilfe und Gynäkologie: Physiologie und Pathologie der Reproduktion. Springer-Verlag. pp. 583–. ISBN 978-3-642-95583-9.
- A. Labhart (6 December 2012). Clinical Endocrinology: Theory and Practice. Springer Science & Business Media. pp. 554–. ISBN 978-3-642-96158-8.
- Horský J, Presl J (1981). "Hormonal Treatment of Disorders of the Menstrual Cycle". In Horsky J, Presl K (eds.). Ovarian Function and its Disorders: Diagnosis and Therapy. Springer Science & Business Media. pp. 309–332. doi:10.1007/978-94-009-8195-9_11. ISBN 978-94-009-8195-9.
- Joachim Ufer (1969). The Principles and Practice of Hormone Therapy in Gynaecology and Obstetrics. de Gruyter. p. 49.
17α-Hydroxyprogesterone caproate is a depot progestogen which is entirely free of side actions. The dose required to induce secretory changes in primed endometrium is about 250 mg. per menstrual cycle.
- Willibald Pschyrembel (1968). Praktische Gynäkologie: für Studierende und Ärzte. Walter de Gruyter. pp. 598, 601. ISBN 978-3-11-150424-7.
- Ferin J (September 1972). "Effects, Duration of Action and Metabolism in Man". In Tausk M (ed.). Pharmacology of the Endocrine System and Related Drugs: Progesterone, Progestational Drugs and Antifertility Agents. Vol. II. Pergamon Press. pp. 13–24. ISBN 978-0080168128. OCLC 278011135.
- Henzl MR, Edwards JA (10 November 1999). "Pharmacology of Progestins: 17α-Hydroxyprogesterone Derivatives and Progestins of the First and Second Generation". In Sitruk-Ware R, Mishell DR (eds.). Progestins and Antiprogestins in Clinical Practice. Taylor & Francis. pp. 101–132. ISBN 978-0-8247-8291-7.
- Janet Brotherton (1976). Sex Hormone Pharmacology. Academic Press. p. 114. ISBN 978-0-12-137250-7.
- Sang GW (April 1994). "Pharmacodynamic effects of once-a-month combined injectable contraceptives". Contraception. 49 (4): 361–85. doi:10.1016/0010-7824(94)90033-7. PMID 8013220.
- Toppozada MK (April 1994). "Existing once-a-month combined injectable contraceptives". Contraception. 49 (4): 293–301. doi:10.1016/0010-7824(94)90029-9. PMID 8013216.
- Bagade O, Pawar V, Patel R, Patel B, Awasarkar V, Diwate S (2014). "Increasing use of long-acting reversible contraception: safe, reliable, and cost-effective birth control" (PDF). World J Pharm Pharm Sci. 3 (10): 364–392. ISSN 2278-4357. Archived from the original (PDF) on 10 August 2017. Retrieved 24 August 2016.
- Goebelsmann U (1986). "Pharmacokinetics of Contraceptive Steroids in Humans". In Gregoire AT, Blye RP (eds.). Contraceptive Steroids: Pharmacology and Safety. Springer Science & Business Media. pp. 67–111. doi:10.1007/978-1-4613-2241-2_4. ISBN 978-1-4613-2241-2.
- Becker H, Düsterberg B, Klosterhalfen H (1980). "[Bioavailability of cyproterone acetate after oral and intramuscular application in men (author's transl)]" [Bioavailability of Cyproterone Acetate after Oral and Intramuscular Application in Men]. Urologia Internationalis. 35 (6): 381–5. doi:10.1159/000280353. PMID 6452729.
- Moltz L, Haase F, Schwartz U, Hammerstein J (May 1983). "[Treatment of virilized women with intramuscular administration of cyproterone acetate]" [Efficacy of Intra muscularly Applied Cyproterone Acetate in Hyperandrogenism]. Geburtshilfe Und Frauenheilkunde. 43 (5): 281–7. doi:10.1055/s-2008-1036893. PMID 6223851.
- Wright JC, Burgess DJ (29 January 2012). Long Acting Injections and Implants. Springer Science & Business Media. pp. 114–. ISBN 978-1-4614-0554-2.
- Chu YH, Li Q, Zhao ZF (April 1986). "Pharmacokinetics of megestrol acetate in women receiving IM injection of estradiol-megestrol long-acting injectable contraceptive". The Chinese Journal of Clinical Pharmacology.
The results showed that after injection the concentration of plasma MA increased rapidly. The meantime of peak plasma MA level was 3rd day, there was a linear relationship between log of plasma MA concentration and time (day) after administration in all subjects, elimination phase half-life t1/2β = 14.35 ± 9.1 days.
- Runnebaum BC, Rabe T, Kiesel L (6 December 2012). Female Contraception: Update and Trends. Springer Science & Business Media. pp. 429–. ISBN 978-3-642-73790-9.
- Artini PG, Genazzani AR, Petraglia F (11 December 2001). Advances in Gynecological Endocrinology. CRC Press. pp. 105–. ISBN 978-1-84214-071-0.
- King TL, Brucker MC, Kriebs JM, Fahey JO (21 October 2013). Varney's Midwifery. Jones & Bartlett Publishers. pp. 495–. ISBN 978-1-284-02542-2.
- Poulin R, Baker D, Poirier D, Labrie F (March 1989). "Androgen and glucocorticoid receptor-mediated inhibition of cell proliferation by medroxyprogesterone acetate in ZR-75-1 human breast cancer cells". Breast Cancer Research and Treatment. 13 (2): 161–72. doi:10.1007/bf01806528. PMID 2525057. S2CID 26116247.
- Brady BM, Anderson RA, Kinniburgh D, Baird DT (April 2003). "Demonstration of progesterone receptor-mediated gonadotrophin suppression in the human male". Clinical Endocrinology. 58 (4): 506–12. doi:10.1046/j.1365-2265.2003.01751.x. PMID 12641635. S2CID 12567639.
- Saleh FM, Grudzinskas AJ, Bradford JM (11 February 2009). Sex Offenders: Identification, Risk Assessment, Treatment, and Legal Issues. Oxford University Press. p. 44. ISBN 978-0-19-517704-6. Archived from the original on 17 June 2014.
- World Health Organization (2009). Stuart MC, Kouimtzi M, Hill SR (eds.). WHO Model Formulary 2008. World Health Organization. p. 368. hdl:10665/44053. ISBN 9789241547659.
- Lothstein, Leslie M. (1996). "Antiandrogen treatment for sexual disorders: Guidelines for establishing a standard of care". Sexual Addiction & Compulsivity. 3 (4): 313–331. doi:10.1080/10720169608400122. ISSN 1072-0162.
- Dangerous Sex Offenders: A Task Force Report of the American Psychiatric Association. American Psychiatric Pub. 1999. pp. 112–144. ISBN 978-0-89042-280-9.
- Kravitz HM, Haywood TW, Kelly J, Liles S, Cavanaugh JL (1996). "Medroxyprogesterone and paraphiles: do testosterone levels matter?". Bull Am Acad Psychiatry Law. 24 (1): 73–83. PMID 8891323.
- Novak E, Hendrix JW, Chen TT, Seckman CE, Royer GL, Pochi PE (October 1980). "Sebum production and plasma testosterone levels in man after high-dose medroxyprogesterone acetate treatment and androgen administration". Acta Endocrinol. 95 (2): 265–70. doi:10.1530/acta.0.0950265. PMID 6449127.
- Kirschner MA, Schneider G (February 1972). "Suppression of the pituitary-Leydig cell axis and sebum production in normal men by medroxyprogesterone acetate (provera)". Acta Endocrinol. 69 (2): 385–93. doi:10.1530/acta.0.0690385. PMID 5066846.
- Asscheman H, Gooren LJ (1993). "Hormone Treatment in Transsexuals". Journal of Psychology & Human Sexuality. 5 (4): 39–54. doi:10.1300/J056v05n04_03. ISSN 0890-7064. S2CID 144580633.
- Meriggiola MC, Gava G (November 2015). "Endocrine care of transpeople part II. A review of cross-sex hormonal treatments, outcomes and adverse effects in transwomen". Clin. Endocrinol. (Oxf). 83 (5): 607–15. doi:10.1111/cen.12754. hdl:11585/541921. PMID 25692882. S2CID 39706760.
- Gooren LJ, Giltay EJ, Bunck MC (January 2008). "Long-term treatment of transsexuals with cross-sex hormones: extensive personal experience". J. Clin. Endocrinol. Metab. 93 (1): 19–25. doi:10.1210/jc.2007-1809. PMID 17986639.
- Deutsch M (17 June 2016). "Guidelines for the Primary and Gender-Affirming Care of Transgender and Gender Nonbinary People" (PDF) (2nd ed.). University of California, San Francisco: Center of Excellence for Transgender Health. p. 28.
- Dahl M, Feldman JL, Goldberg J, Jaberi A (2015). "Endocrine Therapy for Transgender Adults in British Columbia: Suggested Guidelines" (PDF). Vancouver Coastal Health. Retrieved 15 August 2018.
- Leinung MC, Feustel PJ, Joseph J (2018). "Hormonal Treatment of Transgender Women with Oral Estradiol". Transgend Health. 3 (1): 74–81. doi:10.1089/trgh.2017.0035. PMC 5944393. PMID 29756046.
- Onu PE (1995). "Depot medroxyprogesterone in the management of benign prostatic hyperplasia". Eur Urol. 28 (3): 229–35. doi:10.1159/000475056. PMID 8536777.
- Meyer, Walter J.; Walker, Paul A.; Emory, Lee E.; Smith, Edward R. (1985). "Physical, metabolic, and hormonal effects on men of long-term therapy with medroxyprogesterone acetate". Fertility and Sterility. 43 (1): 102–109. doi:10.1016/S0015-0282(16)48326-3. ISSN 0015-0282. PMID 3155506.
- Birrell SN, Hall RE, Tilley WD (January 1998). "Role of the androgen receptor in human breast cancer". Journal of Mammary Gland Biology and Neoplasia. 3 (1): 95–103. doi:10.1023/A:1018730519839. PMID 10819508. S2CID 12044431.
- Buchanan G, Birrell SN, Peters AA, Bianco-Miotto T, Ramsay K, Cops EJ, Yang M, Harris JM, Simila HA, Moore NL, Bentel JM, Ricciardelli C, Horsfall DJ, Butler LM, Tilley WD (September 2005). "Decreased androgen receptor levels and receptor function in breast cancer contribute to the failure of response to medroxyprogesterone acetate". Cancer Research. 65 (18): 8487–96. doi:10.1158/0008-5472.CAN-04-3077. PMID 16166329.
- Rees MC, Hope S, Ravnikar V (12 August 2005). The Abnormal Menstrual Cycle. Taylor & Francis. p. 213. ISBN 978-1-84214-212-7. Archived from the original on 31 December 2013.
- Aronson, JK (20 January 2009). Meyler's Side Effects of Endocrine and Metabolic Drugs. Elsevier. p. 283. ISBN 978-0-444-53271-8. Archived from the original on 31 December 2013.
- Ettinger B, Golditch IM (December 1977). "Medroxyprogesterone acetate for the evaluation of hypertestosteronism in hirsute women". Fertility and Sterility. 28 (12): 1285–8. doi:10.1016/S0015-0282(16)42970-5. PMID 590535.
- Correa de Oliveira RF, Novaes LP, Lima MB, Rodrigues J, Franco S, Khenaifes AI, Francalanci CP (December 1975). "A new treatment for hirsutism". Annals of Internal Medicine. 83 (6): 817–9. doi:10.7326/0003-4819-83-6-817. PMID 1200527.
- Richman RA, Underwood LE, French FS, Van Wyk JJ (December 1971). "Adverse effects of large doses of medroxyprogesterone (MPA) in idiopathic isosexual precocity". The Journal of Pediatrics. 79 (6): 963–71. doi:10.1016/s0022-3476(71)80191-9. PMID 4332067.
- Luciano, A. A. (1992). "Endometriosis—the role of medroxyprogesterone acetate". Journal of Obstetrics and Gynaecology. 12 (sup2): S38–S44. doi:10.3109/01443619209045611. ISSN 0144-3615.
- Nachtigall LE, Raju U, Banerjee S, Wan L, Levitz M (2000). "Serum estradiol-binding profiles in postmenopausal women undergoing three common estrogen replacement therapies: associations with sex hormone-binding globulin, estradiol, and estrone levels". Menopause. 7 (4): 243–50. doi:10.1097/00042192-200007040-00006. PMID 10914617. S2CID 3076514.
- Lundgren S, Lønning PE, Utaaker E, Aakvaag A, Kvinnsland S (June 1990). "Influence of progestins on serum hormone levels in postmenopausal women with advanced breast cancer--I. General findings". J Steroid Biochem. 36 (1–2): 99–104. doi:10.1016/0022-4731(90)90118-c. PMID 2362454.
- Lundgren S, Lønning PE (June 1990). "Influence of progestins on serum hormone levels in postmenopausal women with advanced breast cancer--II. A differential effect of megestrol acetate and medroxyprogesterone acetate on serum estrone sulfate and sex hormone binding globulin". J Steroid Biochem. 36 (1–2): 105–9. doi:10.1016/0022-4731(90)90119-d. PMID 2141886.
- Tomić R, Ljungberg B, Damber JE (1988). "Hormonal effects of high dose medroxyprogesterone acetate treatment in males with renal or prostatic adenocarcinoma". Scand J Urol Nephrol. 22 (1): 15–8. doi:10.1080/00365599.1988.11690377. PMID 2968646.
- Merrin PK, Alexander WD (August 1990). "Cushing's syndrome induced by medroxyprogesterone". BMJ. 301 (6747): 345. doi:10.1136/bmj.301.6747.345-a. PMC 1663616. PMID 2144198.
- Systemic Effects of Oral Glucocorticoids, archived from the original on 28 January 2014
- Ishida Y, Ishida Y, Heersche JN (August 2002). "Pharmacologic doses of medroxyprogesterone may cause bone loss through glucocorticoid activity: an hypothesis". Osteoporos Int. 13 (8): 601–5. doi:10.1007/s001980200080. PMID 12181616. S2CID 23343761.
- Kuhl H (2005). "Pharmacology of estrogens and progestogens: influence of different routes of administration" (PDF). Climacteric. 8 Suppl 1: 3–63. doi:10.1080/13697130500148875. PMID 16112947. S2CID 24616324.
- Sunde A, Rosness PA, Eik-Nes KB (August 1982). "Effects in vitro of medroxyprogesterone acetate on steroid metabolizing enzymes in the rat: selective inhibition of 3 alpha-hydroxysteroid oxidoreductase activity". Journal of Steroid Biochemistry. 17 (2): 197–203. doi:10.1016/0022-4731(82)90122-4. PMID 6213817.
- Penning TM, Sharp RB, Krieger NR (December 1985). "Purification and properties of 3 alpha-hydroxysteroid dehydrogenase from rat brain cytosol. Inhibition by nonsteroidal anti-inflammatory drugs and progestins". The Journal of Biological Chemistry. 260 (28): 15266–72. doi:10.1016/S0021-9258(18)95730-3. PMID 2933398.
- Pazol K, Wilson ME, Wallen K (June 2004). "Medroxyprogesterone acetate antagonizes the effects of estrogen treatment on social and sexual behavior in female macaques". The Journal of Clinical Endocrinology and Metabolism. 89 (6): 2998–3006. doi:10.1210/jc.2003-032086. PMC 1440328. PMID 15181090.
- Meyer L, Venard C, Schaeffer V, Patte-Mensah C, Mensah-Nyagan AG (April 2008). "The biological activity of 3alpha-hydroxysteroid oxido-reductase in the spinal cord regulates thermal and mechanical pain thresholds after sciatic nerve injury". Neurobiology of Disease. 30 (1): 30–41. doi:10.1016/j.nbd.2007.12.001. PMID 18291663. S2CID 5830825.
- Mellon SH, Griffin LD (2002). "Neurosteroids: biochemistry and clinical significance". Trends in Endocrinology and Metabolism. 13 (1): 35–43. doi:10.1016/s1043-2760(01)00503-3. PMID 11750861. S2CID 11605131.
- Lee TC, Miller WL, Auchus RJ (June 1999). "Medroxyprogesterone acetate and dexamethasone are competitive inhibitors of different human steroidogenic enzymes". The Journal of Clinical Endocrinology and Metabolism. 84 (6): 2104–10. doi:10.1210/jcem.84.6.5646. PMID 10372718.
- Söderpalm AH, Lindsey S, Purdy RH, Hauger R, Wit de H (April 2004). "Administration of progesterone produces mild sedative-like effects in men and women". Psychoneuroendocrinology. 29 (3): 339–54. doi:10.1016/s0306-4530(03)00033-7. PMID 14644065. S2CID 21796848.
- McAuley JW, Kroboth PD, Stiff DD, Reynolds IJ (May 1993). "Modulation of [3H]flunitrazepam binding by natural and synthetic progestational agents". Pharmacology Biochemistry and Behavior. 45 (1): 77–83. doi:10.1016/0091-3057(93)90089-c. PMID 8516376. S2CID 42764270.
- Weizman A (1 February 2008). Neuroactive Steroids in Brain Function, Behavior and Neuropsychiatric Disorders: Novel Strategies for Research and Treatment. Springer Science & Business Media. pp. 104, 107, 112. ISBN 978-1-4020-6854-6.
- Hofbauer KG, Anker SD, Inui A, Nicholson JR (22 December 2005). Pharmacotherapy of Cachexia. CRC Press. pp. 292–. ISBN 978-1-4200-4895-7.
Medroxyprogesterone [acetate] has similarly been shown to increase appetite and food intake with stabilization of body weight at a dose of 1000 mg (500 mg twice daily).13 Although the drug may be used at 500 to 4000 mg daily, side effects increase above oral doses of 1000 mg daily.16
- Doyle D, Hanks G, Cherny NI (3 February 2005). Oxford Textbook Of Palliative Medicine. Oxford University Press. p. 553. ISBN 978-0-19-856698-4. Archived from the original on 18 June 2013.
- Neubauer H, Ma Q, Zhou J, Yu Q, Ruan X, Seeger H, Fehm T, Mueck AO (October 2013). "Possible role of PGRMC1 in breast cancer development". Climacteric. 16 (5): 509–13. doi:10.3109/13697137.2013.800038. PMID 23758160. S2CID 29808177.
- Trabert B, Sherman ME, Kannan N, Stanczyk FZ (September 2019). "Progesterone and breast cancer". Endocr. Rev. 41 (2): 320–344. doi:10.1210/endrev/bnz001. PMC 7156851. PMID 31512725.
- Stanczyk, Frank Z.; Bhavnani, Bhagu R. (2014). "Use of medroxyprogesterone acetate for hormone therapy in postmenopausal women: Is it safe?". The Journal of Steroid Biochemistry and Molecular Biology. 142: 30–38. doi:10.1016/j.jsbmb.2013.11.011. ISSN 0960-0760. PMID 24291402. S2CID 22731802.
- Victor, Arne; Johansson, Elof D.B. (1976). "Pharmacokinetic observations on medroxyprogesterone acetate administered orally and intravaginally". Contraception. 14 (3): 319–329. doi:10.1016/0010-7824(76)90099-8. ISSN 0010-7824. PMID 975821.
- Hiroi, M.; Stanczyk, F.Z.; Goebelsmann, U.; Brenner, P.F.; Lumkin, M.E.; Mishell, D.R. (1975). "Radioimmunoassay of serum medroxyprogesterone acetate (Provera ) in women following oral and intravaginal administration". Steroids. 26 (3): 373–386. doi:10.1016/0039-128X(75)90082-3. ISSN 0039-128X. PMID 1198624. S2CID 24777672.
- Svensson, L.-O.; Johnson, S.Hedman; Olsson, S.-E. (1994). "Plasma concentrations of medroxyprogesterone acetate, estradiol and estrone following oral administration of Klimaxil, Trisequence / Provera and Divina. A randomized, single-blind, triple cross-over bioavailability study in menopausal women". Maturitas. 18 (3): 229–238. doi:10.1016/0378-5122(94)90129-5. ISSN 0378-5122. PMID 8015506.
- Järvinen, Asko; Kainulainen, Petri; Nissilä, Minna; Nikkanen, Hanna; Kela, Marjo (2004). "Pharmacokinetics of estradiol valerate and medroxyprogesterone acetate in different age groups of postmenopausal women". Maturitas. 47 (3): 209–217. doi:10.1016/j.maturitas.2003.01.001. ISSN 0378-5122. PMID 15036491.
- "Medroxyprogesterone Acetate - Drug Summary". Prescribers' Digital Reference (PDR). ConnectiveRx. Archived from the original on 7 October 2018. Retrieved 17 June 2019.
When needed, tablets may be administered sublingually†; absorption is adequate by this route.
- Sutton, Frank D. (1975). "Progesterone for Outpatient Treatment of Pickwickian Syndrome". Annals of Internal Medicine. 83 (4): 476–9. doi:10.7326/0003-4819-83-4-476. ISSN 0003-4819. PMID 1101759.
The sublingual route was chosen to avoid any irregular absorption that might result from simultaneous food intake.
- Jain J, Kwan D, Forcier M (April 2019). "Medroxyprogesterone Acetate in Gender-Affirming Therapy for Transwomen: Results from a Retrospective Study". The Journal of Clinical Endocrinology & Metabolism. 104 (11): 5148–5156. doi:10.1210/jc.2018-02253. ISSN 0021-972X. PMID 31127826.
- van Hoogdalem EJ, de Boer AG, Breimer DD (August 1991). "Pharmacokinetics of rectal drug administration, Part II. Clinical applications of peripherally acting drugs, and conclusions". Clin Pharmacokinet. 21 (2): 110–28. doi:10.2165/00003088-199121020-00003. PMID 1884566. S2CID 11720029.
- Mishell DR (May 1996). "Pharmacokinetics of depot medroxyprogesterone acetate contraception". The Journal of Reproductive Medicine. 41 (5 Suppl): 381–90. PMID 8725700.
- Sang GW (April 1994). "Pharmacodynamic effects of once-a-month combined injectable contraceptives". Contraception. 49 (4): 361–85. doi:10.1016/0010-7824(94)90033-7. PMID 8013220.
- Garza-Flores J, Hall PE, Perez-Palacios G (1991). "Long-acting hormonal contraceptives for women". J. Steroid Biochem. Mol. Biol. 40 (4–6): 697–704. doi:10.1016/0960-0760(91)90293-e. PMID 1958567. S2CID 26021562.
- Gabelnick, Henry L.; Hall, Peter E. (1987). "Long-acting methods for fertility regulation". Journal of Controlled Release. 6 (1): 387–394. doi:10.1016/0168-3659(87)90092-7. ISSN 0168-3659.
- Antal, E; Dick, C; Wrightiii, C; Welshman, I; Block, E (1989). "Comparative bioavailability of two medroxyprogesterone acetate suspensions". International Journal of Pharmaceutics. 54 (1): 33–39. doi:10.1016/0378-5173(89)90162-2. ISSN 0378-5173.
- Ishihara M, Kirdani Y, Osawa Y, Sandberg AA (January 1976). "The metabolic fate of medroxyprogesterone acetate in the baboon". Journal of Steroid Biochemistry. 7 (1): 65–70. doi:10.1016/0022-4731(76)90167-9. PMID 1271819.
- DeVita VT, Lawrence TS, Rosenberg SA (7 January 2015). DeVita, Hellman, and Rosenberg's Cancer: Principles & Practice of Oncology. Wolters Kluwer Health. pp. 1149–. ISBN 978-1-4698-9455-3.
- Goebelsmann, Uwe (1986). "Pharmacokinetics of Contraceptive Steroids in Humans". In A. T. Gregoire; Richard P. Blye (eds.). Contraceptive Steroids: Pharmacology and Safety. Springer Science & Business Media. pp. 67–111. doi:10.1007/978-1-4613-2241-2_4. ISBN 978-1-4613-2241-2.
- Ortiz A, Hirol M, Stanczyk FZ, Goebelsmann U, Mishell DR (January 1977). "Serum medroxyprogesterone acetate (MPA) concentrations and ovarian function following intramuscular injection of depo-MPA". J. Clin. Endocrinol. Metab. 44 (1): 32–8. doi:10.1210/jcem-44-1-32. PMID 833262.
- Fotherby K, Koetsawang S, Mathrubutham M (November 1980). "Pharmacokinetic study of different doses of Depo Provera". Contraception. 22 (5): 527–36. doi:10.1016/0010-7824(80)90105-5. PMID 6451351.
- Elks J (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. p. 657. ISBN 978-1-4757-2085-3. Archived from the original on 5 November 2017.
- Ademuyiwa FO, Miller KD (December 2008). "Incorporation of antiangiogenic therapies in the treatment of metastatic breast cancer". Clin. Breast Cancer. 8 Suppl 4: S151–6. doi:10.3816/CBC.2008.s.011. PMID 19158035.
- "FMPA - AdisInsight". adisinsight.springer.com.
- FR 1295307, "Procédé de préparation de dérivés cyclopentano-phénanthréniques", published 8 June 1962, assigned to Syntex SA
- US granted 3377364, Spero G, "6-methyl-17alpha-hydroxyprogesterone, the lower fatty acid 17-acylates and methods for producing the same", published 9 April 1968, assigned to Upjohn Company
- Green W (1987). "Odyssey of Depo-Provera: Contraceptives, Carcinogenic Drugs, and Risk-Management Analyses". The. Food Drug Cosm. LJ. Chicago (42): 567–587.
Depo-Provera is a drug, manufactured by The Upjohn Co., whose active ingredient is medroxyprogesterone acetate (MPA). FDA first approved the drug in 1959 to treat amenorrhea,5 irregular uterine bleeding, and threatened and habitual abortion.
- Hartmann KE, Jerome RN, Lindegren ML, Potter SA, Shields TC, Surawicz TS, Andrews JC (2013). Primary Care Management of Abnormal Uterine Bleeding. Agency for Healthcare Research and Quality (US). PMID 23617013.
- Gelijns A (1991). Innovation in Clinical Practice: The Dynamics of Medical Technology Development. National Academies. pp. 167–. NAP:13513.
- William Andrew Publishing (22 October 2013). Pharmaceutical Manufacturing Encyclopedia. Elsevier. pp. 1501–. ISBN 978-0-8155-1856-3.
- Kolbe HK (1976). Population/fertility control thesaurus (PDF). Population Information Program, Science Communication Division, Dept. of Medical and Public Affairs, George Washington University. Archived (PDF) from the original on 9 October 2016.
- Bolivar De Lee J (1966). The ... Year Book of Obstetrics and Gynecology. Year Book Publishers. p. 339.
One of these is medroxyprogesterone acetate, which is sold in the United States by Upjohn as Provest, and is obtainable abroad as Provestral, Provestrol, Cyclo-Farlutal, and the more frankly suggestive Nogest.
- Fínkelstein M (1966). Research on Steroids. Pergamon. pp. 469, 542.
- Christopher Li (11 November 2009). Breast Cancer Epidemiology. Springer Science & Business Media. pp. 110–. ISBN 978-1-4419-0685-4.
- Levitt JI (30 April 2015). Black Women and International Law: Deliberate Interactions, Movements and Actions. Cambridge University Press. pp. 230–231. ISBN 978-1-316-29840-4.
- Documentation on Women's Concerns. Library and Documentation Centre, All India Association for Christian Higher Education. January 1998.
Upjohn meanwhile, had been repeatedly seeking FDA approval for use of DMPA as a contraceptive, but applications were rejected in 1967, 1978 and yet again in 1983, [...]
- Shoupe D, Mishell DR (28 September 2015). The Handbook of Contraception: A Guide for Practical Management. Humana Press. pp. 126–. ISBN 978-3-319-20185-6.
- Morton I, Hall JM (31 October 1999). Concise Dictionary of Pharmacological Agents: Properties and Synonyms. Springer Science & Business Media. pp. 173–. ISBN 978-0-7514-0499-9.
- Louisiana State Legislature. "§43.6. Administration of medroxyprogesterone acetate (MPA) to certain sex offenders". Louisiana Revised Statutes. Retrieved 8 July 2019.
- Unzeitig V, van Lunsen RH (15 February 2000). Contraceptive Choices and Realities: Proceedings of the 5th Congress of the European Society of Contraception. CRC Press. pp. 73–. ISBN 978-1-85070-067-8.
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans; World Health Organization; International Agency for Research on Cancer (2007). Combined Estrogen-progestogen Contraceptives and Combined Estrogen-progestogen Menopausal Therapy. World Health Organization. p. 44. ISBN 978-92-832-1291-1.
- John David Gordon (2007). Obstetrics, Gynecology & Infertility: Handbook for Clinicians. Scrub Hill Press, Inc. pp. 228–. ISBN 978-0-9645467-7-6.
- "Contraceptives. Case for public enquiry". Economic and Political Weekly. 29 (15): 825–6. 1994. Popline database document number 096527.
- Sorojini, NB (January–March 2005). "Why women's groups oppose injectable contraceptives". Indian Journal of Medical Ethics. 13 (1). Archived from the original on 6 May 2006.
- "Reference Manual for Injectable Contraceptive (MPA)" (PDF). nhm.gov.in. Retrieved 26 February 2020.
- Madeline Boscoe (6 December 1991). "Canadian Coalition on Depo-Provera letter to The Honorable Benoit Bouchard, National Minister of Health and Welfare". Canadian Women's Health Network. Archived from the original on 5 February 2007. Retrieved 22 August 2006.
- "Class action suit filed over birth control drug". CTV.ca. 19 December 2005. Archived from the original on 13 August 2006. Retrieved 22 August 2006.
- ""Israeli minister appointing team to probe Ethiopian birth control shot controversy". Haaretz. Archived from the original on 20 June 2015. Retrieved 20 June 2015.
- Leary WE (October 1992). "U.S. approves injectable drug as birth control". The New York Times on the Web: A1, A14. PMID 11646958. Archived from the original on 8 December 2008.
- "Progestins (IARC Summary & Evaluation, Supplement7, 1987)". Archived from the original on 7 November 2017. Retrieved 15 October 2016.
- Amy Goodman (February–March 1985). "The Case Against Depo-Provera - Problems in the U.S". Multinational Monitor. 6 (2 & 3). Archived from the original on 3 October 2006.
- "Controversy over Depo-Provera". Washington Drug & Device Letter. 9 (1): 2. January 1977. PMID 12335988.
- Thomas DB, Ye Z, Ray RM (January 1995). "Cervical carcinoma in situ and use of depot-medroxyprogesterone acetate (DMPA). WHO Collaborative Study of Neoplasia and Steroid Contraceptives". Contraception. 51 (1): 25–31. doi:10.1016/0010-7824(94)00007-J. PMID 7750280.
- "Depot-medroxyprogesterone acetate (DMPA) and risk of invasive squamous cell cervical cancer. The WHO Collaborative Study of Neoplasia and Steroid Contraceptives". Contraception. 45 (4): 299–312. April 1992. doi:10.1016/0010-7824(92)90052-U. PMID 1387601.
- Thomas DB, Ray RM (November 1995). "Depot-medroxyprogesterone acetate (DMPA) and risk of invasive adenocarcinomas and adenosquamous carcinomas of the uterine cervix. WHO Collaborative Study of Neoplasia and Steroid Contraceptives". Contraception. 52 (5): 307–12. doi:10.1016/0010-7824(95)00215-V. PMID 8585888.
- Shapiro S, Rosenberg L, Hoffman M, Kelly JP, Cooper DD, Carrara H, Denny LE, du Toit G, Allan BR, Stander IA, Williamson AL (June 2003). "Risk of invasive cancer of the cervix in relation to the use of injectable progestogen contraceptives and combined estrogen/progestogen oral contraceptives (South Africa)". Cancer Causes & Control. 14 (5): 485–95. doi:10.1023/A:1024910808307. PMID 12946044. S2CID 34683749.
- Kaunitz AM (May 1996). "Depot medroxyprogesterone acetate contraception and the risk of breast and gynecologic cancer". The Journal of Reproductive Medicine. 41 (5 Suppl): 419–27. PMID 8725705.
- Hawkins K, Elliott J (5 May 1996). "Seeking Approval". Albion Monitor. Archived from the original on 21 November 2015. Retrieved 20 November 2006.
- "Sterilization of minors leads to controversy". Family Planning/Population Reporter; A Review of State Laws and Policies. 2 (4): 77–8. August 1973. PMID 12257656.
- Egan TM, Siegert RJ, Fairley NA (August 1993). "Use of hormonal contraceptives in an institutional setting: reasons for use, consent and safety in women with psychiatric and intellectual disabilities". The New Zealand Medical Journal. 106 (961): 338–41. PMID 8341476.
- Singh S (May 1995). "Adolescent knowledge and use of injectable contraceptives in developing countries". The Journal of Adolescent Health. 16 (5): 396–404. doi:10.1016/S1054-139X(94)00060-R. PMID 7662691.
- "Clinicians clash with consumer groups over possible Depo ban". Contraceptive Technology Update. 16 (1): 11–4. January 1995. PMID 12319319.
- Toppozada M (June 1977). "The clinical use of monthly injectable contraceptive preparations". Obstet Gynecol Surv. 32 (6): 335–47. doi:10.1097/00006254-197706000-00001. PMID 865726.
- Joseph William Goldzieher; Kenneth Fotherby (1994). Pharmacology of the contraceptive steroids. Raven Press. p. 154. ISBN 978-0-7817-0097-9.
- Zañartu J, Rice-Wray E, Goldzieher JW (October 1966). "Fertility control with long-acting injectable steroids. A preliminary report". Obstet Gynecol. 28 (4): 513–5. PMID 5925038.
- Harry Beckman (1967). The Year Book of Drug Therapy. Year Book Publishers.
- Piotrowski Z, Greenberg RE (2016). "Antiandrogen Monotherapy in the Treatment of Prostate Cancer". Prostate Cancer. pp. 515–521. doi:10.1016/B978-0-12-800077-9.00055-4. ISBN 9780128000779.
- Forster TH, Stoffel F, Gasser TC (2002). "Hormone therapy in advanced prostate cancer". Front Radiat Ther Oncol. Frontiers of Radiation Therapy and Oncology. 36: 49–65. doi:10.1159/000061329. ISBN 3-8055-7217-4. PMID 11842755.
- Newling DW (March 1997). "The palliative therapy of advanced prostate cancer, with particular reference to the results of recent European clinical trials". Br J Urol. 79 Suppl 1: 72–81. doi:10.1111/j.1464-410X.1997.tb00805.x. PMID 9088277.
- Denis LJ, Griffiths K, Kaisary AV, Murphy GP (1 March 1999). Textbook of Prostate Cancer: Pathology, Diagnosis and Treatment: Pathology, Diagnosis and Treatment. CRC Press. pp. 296–. ISBN 978-1-85317-422-3.
- Nieschlag E (2010). "Clinical trials in male hormonal contraception" (PDF). Contraception. 82 (5): 457–70. doi:10.1016/j.contraception.2010.03.020. PMID 20933120.
- "Medroxyprogesterone - InKine - AdisInsight".
- Srinivasan R, Lichtenstein GR (April 2004). "Recent developments in the pharmacological treatment of Crohn's disease". Expert Opin Investig Drugs. 13 (4): 373–91. doi:10.1517/13543784.13.4.373. PMID 15102587. S2CID 22533823.
- Saxena, Ashwini; Scaini, Giselli; Bavaresco, Daniela V.; Leite, Camila; Valvassoria, Samira S.; Carvalho, André F.; Quevedo, João (2017). "Role of Protein Kinase C in Bipolar Disorder: A Review of the Current Literature". Molecular Neuropsychiatry. 3 (2): 108–124. doi:10.1159/000480349. ISSN 2296-9209. PMC 5701269. PMID 29230399.
- Simpson BS, Papich MG (March 2003). "Pharmacologic management in veterinary behavioral medicine". Vet. Clin. North Am. Small Anim. Pract. 33 (2): 365–404, vii. doi:10.1016/S0195-5616(02)00130-4. PMID 12701517.
External links
- "Medroxyprogesterone acetate". Drug Information Portal. U.S. National Library of Medicine.